Systolic murmur is a murmur heard during the period of contraction of the ventricles between the first and second ventricles.
Hemodynamic changes in cardiovascular system cause the transformation of layered blood flow into a vortex, which causes vibration of the surrounding tissue, conducted to the surface chest and perceived as sound phenomena in the form of systolic murmur.
The presence of an obstruction or narrowing in the blood flow is of decisive importance for the occurrence of vortex movements and the appearance of systolic murmur, and the strength of the systolic murmur is not always proportional to the degree of narrowing. A decrease in blood viscosity, for example in anemia, creates conditions that facilitate the occurrence of systolic murmur.
Systolic murmurs are divided into inorganic, or functional, and organic, caused by morphological changes in the heart and valvular apparatus.
TO functional systolic murmurs include: 1) systolic murmur of relative mitral insufficiency, heard above the apex of the heart; 2) systolic murmur over the aorta during its expansion; 3) systolic murmur with aortic valve insufficiency; 4) systolic murmur above pulmonary artery when it expands; 5) systolic murmur, which occurs during nervous excitement or significant physical stress, heard at the base (and sometimes above the apex) of the heart along with increased sonority of tones;
6) systolic murmur during fever, sometimes found over the aorta and pulmonary artery; 7) systolic murmur with severe anemia and, audible over the entire region of the heart.
Systolic murmur, which occurs when the aorta or pulmonary artery dilates, is associated with a relative narrowing of the mouths of these vessels and is most loud at the very beginning of systole, which distinguishes it from systolic murmur with organic stenosis. Systolic murmur in aortic valve insufficiency depends on the increase in left ventricular stroke volume and the rate of blood ejection through the relatively narrowed aortic ostium.
In addition, functional systolic murmurs include the so-called physiological systolic murmur, often heard in young healthy people at the base and sometimes at the apex of the heart. Physiological systolic murmur over the pulmonary artery can be heard in healthy people aged 17-18 years in 30% of cases, mainly in people of asthenic physique. This noise is heard only in a limited area, changes depending on the position of the body, breathing and pressure with a stethoscope, has a quiet, blowing character, and is detected more often at the beginning of systole.
Organic systolic murmurs for valve defects, they are divided into ejection murmurs (aortic or pulmonary artery) and murmurs (bicuspid or tricuspid valve insufficiency).
The systolic murmur of aortic stenosis is rough and strong, heard in the second right intercostal space at the sternum and extends upward to the right clavicle and neck arteries; at the place of listening and at carotid arteries systolic is palpated; murmur occurs after the first tone, the intensity of the murmur increases towards mid-systole. In the case of severe stenosis, the maximum noise occurs in the second half of systole due to slow expulsion of blood. Systolic murmur with dilatation of the sclerotic aorta is not so rough, there is no systolic tremor, the maximum murmur is determined at the beginning of systole, and the second tone is sonorous or amplified. In elderly people with atherosclerosis, in addition to the systolic murmur over the aorta, a systolic murmur over the apex of the heart can be heard - the so-called aortomitral systolic murmur.
When the mouth of the pulmonary artery is narrowed, a systolic murmur is heard in the second intercostal space on the left; the noise is rough, strong, extends to the left clavicle, accompanied by systolic trembling at the site of auscultation; the second sound is bifurcated with the pulmonary component located before the aortic one. With sclerosis and dilatation of the pulmonary artery, the maximum systolic murmur is heard at the beginning of systole, the second tone is usually significantly enhanced. Sometimes a systolic murmur is heard over the pulmonary artery when the interatrial septum is not closed as a result of expansion of the initial part of the pulmonary artery; in this case, the second tone is usually bifurcated.
When the interventricular septum is not closed due to the passage of blood through a small defect from the left to the right ventricle, a rough and loud systolic murmur appears in the third and fourth intercostal spaces on the left at the sternum, sometimes with a distinct systolic tremor.
Systolic murmur with insufficiency mitral valve best heard above the apex, extending to the axillary region; a blowing murmur that begins immediately after the first sound and weakens towards the end of systole.
Systolic murmur with tricuspid valve insufficiency is heard in the lower part of the sternum; it is often very quiet and difficult to distinguish from the coexisting systolic murmur of mitral origin.
Systolic murmur with coarctation of the aorta is heard at the base of the heart, the aorta and pulmonary artery, but it is often louder on the back in the area of the left suprascapular fossa, spreading along; the noise begins some time after the first tone and may end after the second tone. With a patent ductus arteriosus, the murmur is systolic and diastolic due to the flow of blood from the aorta to the pulmonary artery during both cardiac cycles; The murmur is best heard over the pulmonary artery or under the left clavicle.
If a persistent systolic murmur is detected, the patient should be referred to a doctor for a thorough examination.
15-12-2016 at 23:41Time is running. I won't say that I'm a disciplined blogger. Disciplined bloggers produce at least three articles per week. I do it less often, because, on the one hand, I’m always busy. On the other hand, most of my messages require serious preliminary research, often several dozen pages of professional text. Nevertheless, . It's time to talk about noise.
Systolic murmurs, to start.
There are two approaches in medicine. Or rather, there are two types of medical authors, my friend.
The first value common sense and logic: etiology→pathogenesis→clinic→treatment→prognosis. Knowing the theory, you have the opportunity, based on a small number of facts, to complete and predict reality, sometimes a very complex reality. For example, based on the characteristics of hemodynamic noise and pulse properties, assume the presence of a specific valve defect and its severity.
The second say that this is, they say, unreliable, they say, there are no randomized studies. Like, just the facts. And there must be r<0,05. И вместо теорий начинают навязывать свои таблицы.
This kills logic and system. True, on the other hand, it gives rise to such pearls as “the probability of disease X is higher if such a diagnosis has already been made for this patient before, sensitivity, specificity, etc.” Seriously: they write this. If this patient has already been diagnosed with disease X before, then this is a good predictor (read “predictor”, predictor!) that disease X still exists. Science has come far, it’s just mysticism!
Fortunately, I am definitely one of the first. I respect common sense and time-tested facts.
Why am I talking about this? Because the recently deceased British cardiologist AUBREY LEATHAM unfairly came under criticism. This man did a lot for cardiology, in particular for the development of cardiac auscultation and phonocardiography, in the last century. I will probably return to this criticism later (they will regret it). And now about the AUBREY LEATHAM approach. It is very simple and makes it easy to understand most systolic murmurs.
Most systolic murmurs are divided into two types:
- midsystolic or ejection murmurs
- pansystolic or regurgitant murmurs
Origin of noise
Ejection murmurs are associated with the expulsion of blood from the ventricles through the natural outflow tract. These may be normal semilunar valves, stenotic semilunar valves, or possibly expulsion of blood through subvalvular or supravalvular stenosis. Otherwise: the noise is associated with the expulsion of blood from the ventricles through the natural outflow pathway, narrowed or not.
Pansystolic regurgitation murmurs are associated with only three conditions:
- mitral regurgitation
- tricuspid regurgitation
- ventricular septal defect
What is the difference between the two types of noise?
Midsystolic ejection murmurs have an increasing and decreasing, as if spindle-shaped, shape. The peak of the noise occurs in the first third or middle of systole. These noises end before the second tone.
Even more interesting: these noises always end before the corresponding component of the second tone. For example, the murmur of pulmonary stenosis may end after the aortic component of the second sound, but before the onset of the pulmonary component of the second sound. Remember that in pulmonary stenosis the second sound is widely split. The aortic component of the second sound in this case may be buried in the systolic murmur, but the pulmonary component will be heard after a short pause after the end of the murmur.
This occurs because the peak ejection of blood from the ventricles occurs approximately in mid-systole. Further, the intensity of blood flow and, accordingly, the volume of the noise decreases and ends before the closure of the semilunar valves.
Pansystolic regurgitant murmurs the volume is almost uniform throughout the entire systole. They come close to the second tone. But they don’t necessarily start with the first tone. They can begin at any time during systole. Why? Because in the atria, compared to the ventricles, the pressure in systole is much lower. Therefore, a high pressure gradient between the ventricles and atria remains throughout systole. Regurgitation murmurs may even continue for a short time after the second sound. Indeed, at the moment the semilunar valves close, the pressure in the ventricles is much higher than in the atria. So when antegrade blood flow through the semilunar valves is stopped and they close, the pressure in the ventricles is much higher than in the atria, and the regurgitant flow, as well as the murmur, persists for a short time after the closure of the semilunar valves and the second sound is heard.
After a long pause, I continue the tutorial on cardiac auscultation.
Here I will describe auscultatory symptoms of mitral valve prolapse, which are not usually written about in cardiology manuals. It’s not that difficult to come across such a picture; it’s not uncommon. Becoming familiar with these symptoms will save you from diagnostic confusion. Which I had more than once, by the way.

Male between 60 and 70 years old. Complaints of shortness of breath with light exertion. When walking, he sometimes feels like he might faint. The condition progressively worsens for about six months. Echocardiography absolutely accurately identified the cause of poor health: left atrial myxoma.
Is it possible to detect left atrial myxoma by auscultation of the heart?
01/30/2016 at 23:42 08-02-2015 at 21:02Aubrey Leatham (pictured) did a lot to study the second tone in the middle of the last century and is the author of the metaphor that sounds in the title of this article. I don’t know how he argued this, since I couldn’t find an article where it was said (Leatham A. The second heart sound: Key to auscultation of the heart. Acta Cardiol. 1964; 19:395). I'll write on my own behalf.

The second episode of an action-packed miniseries in which I try to squeeze into a minimum of time everything a clinician needs to know about one of the most common and valuable auscultatory symptoms in cardiology: gallops. He gave several audio examples with synchronous display of phonocardiograms. The sound was adapted for simple computer audio speakers. In life, the tones of gallops are muffled.
In this series, the third tone and T3 gallop. The third tone is a grave-sinister symptom.
18-10-2014 at 14:23
I continue publishing.
The last type of splitting of the second tone is paradoxical splitting. With paradoxical, or reverse splitting of the second tone, the latter splits not on inhalation, but on exhalation. On inspiration, the splitting interval decreases until the splitting disappears.
This is the only option for splitting the second sound, when the aortic component follows the pulmonary one. During inspiration, the pulmonary component is deposited and “catches up” with the aortic component (see figure). The aortic component tends to occur earlier during inspiration and moves toward the pulmonary component.

T1 is the first sound, P2 is the pulmonary component, A2 is the aortic component of the second sound.
The only mechanism for the formation of reverse splitting of the second tone is the delay of the aortic component. The causes may be electrical (due to abnormal function of the cardiac conduction system) or hemodynamic.
28-09-2014 at 15:58I continue publishing my own.
Now is the time to examine in detail the scenarios for splitting the second tone. Let's start with persistent splitting, in which the second tone is split both on inhalation and exhalation. In this case, during inhalation, the splitting interval increases (see figure). Usually the splitting interval is greater than normal, the first component is aortic, the second is pulmonary.
1. The first tone is heard after a long pause, the second tone - after a short one.
2. The first tone is longer (on average 0.11 s), the second tone is shorter (0.07 s.)
3. I tone is lower, II tone is higher.
4. The first sound coincides in time with the apical impulse and with the pulse in the carotid artery.
When auscultating heart sounds, it is necessary to characterize the number of tones, their rhythm, volume, sound integrity. When additional tones are identified, their auscultatory features are noted: relation to the phases of the cardiac cycle, volume, timbre.
Heart sounds can be rhythmic or arrhythmic if the patient has a heart rhythm disorder (extrasystole, atrial fibrillation, etc.). Special auscultatory rhythms (quail rhythm, gallop rhythm) can also be heard.
The volume of tones is estimated based on the ratio of the sound volume of tones I and II at various points.
The volume of the first tone is characterized at the mitral and tricuspid valves, i.e. on those valves that participate in its formation. The volume of the first tone is considered normal if it sounds 1.5-2 times louder than the second tone. If the first tone is heard 3-4 times louder than the second tone, this is regarded as an increase in the first tone. If the 1st tone is the same in volume as the 2nd tone or is quieter than it, the 1st tone is weakened.
The volume of the second tone is characterized in the aorta and pulmonary trunk. Moreover, in a healthy person, the volume of the second tone at these points prevails over the volume of the first tone by 1.5-2 times. In addition, the volume of tone II at the listening points of these two valves is the same. If the second tone is heard louder on the aorta or pulmonary trunk, then this condition is characterized as an accent of the second tone on one or another valve.
The volume of heart sounds may depend on the conditions under which sound vibrations are conducted.
Evenly decrease the volume of both tones above the apex of the heart while maintaining the predominance of the first tone is usually associated with noncardiac causes: accumulation of air or fluid in the left pleural cavity, pulmonary emphysema, effusion into the pericardial cavity, obesity.
Attenuation of both tones occurs when the heart muscle is damaged (myocarditis, cardiosclerosis, myocardial infarction).
Boosting both tones observed during physical activity, fever, agitation, thyrotoxicosis, in the initial stages of anemia, and compaction of lung tissue.
The main reasons for the weakening of the first tone above the apex are:
Mitral valve insufficiency (decreased amplitude of movement of deformed valve leaflets, absence of a period of closed valves);
Damage to the heart muscle with weakening of the contractility of the left ventricle due to weakening of the muscle component (myocarditis, myocardial infarction, myocardial dystrophy, dilated myocardiopathy);
Increased diastolic filling of the left ventricle (mitral valve insufficiency, aortic valve insufficiency);
Slowing down of contraction of the left ventricle with its pronounced hypertrophy (aortic defects, hypertension).
Weakening of the first tone at the xiphoid process occurs with tricuspid valve insufficiency due to weakening of the valve component, with pulmonary valve insufficiency due to weakening of the muscle component.
Strengthening the first tone at the apex observed with stenosis of the left atrioventricular orifice, as well as with tachycardia and extrasystole, due to low diastolic filling of the ventricles. In patients with complete atrioventricular block, a sudden significant increase in the first sound is periodically heard (Strazhesko's "cannon tone") against the background of pronounced bradycardia, which is explained by the random coincidence of contractions of the atria and ventricles.
Weakening of the second tone over the aorta occurs with aortic valve insufficiency and low blood pressure.
Weakening of the second tone over the pulmonary trunk occurs when the pulmonary valve is insufficient.
Strengthening of the II tone (emphasis of the II tone) over the aorta observed with high blood pressure, or with atherosclerotic thickening of the aortic wall.
Increased P tone (P tone accent) above the pulmonary trunk sometimes normally heard in young people, in older people it is observed with increased pressure in the pulmonary circulation (chronic pulmonary pathology, mitral defects).
When the heart rate changes (pronounced tachycardia), the duration of the systolic and diastolic pauses are approximately equal, a peculiar heart melody appears, similar to the rhythm of a pendulum - pendulum rhythm(with equal volumes of I and II tones) or resembling the fetal heartbeat - embryocardia (I tone is louder than II tone).
In some pathological conditions, above the apex of the heart, along with the main tones, additional, or extratones. Such extratones can be detected in systole and diastole. Diastolic extratones include sounds III and IV, as well as the sound of the mitral valve opening.
Additional III and IV sounds appear with myocardial damage. Their formation is caused by reduced resistance of the walls of the ventricles, which leads to abnormal vibration during rapid filling of the ventricles with blood at the beginning of diastole (III sound) and during atrial systole, at the end of diastole (IV sound). These extratones are usually quiet, short, low, and are often combined with a weakening of the first tone at the apex and tachycardia, which creates a unique three-part melody - a gallop rhythm.
Normally, the third tone can be heard in thin people under the age of 20.
In pathology in adults, the physiological third tone intensifies and then the melody of a three-part rhythm appears - protodiastolic "gallop rhythm" .
In children under 6 years of age, a sound (IV tone) may be heard before the first sound, which is caused by the rapid entry of blood into the ventricles from the atria during their contraction.
In adults, the appearance of the IV tone creates a pathological presystolic “gallop rhythm”. Presystolic "gallop rhythm" observed when atrioventricular conduction slows. In this case, there is a significant pause between the sound caused by contraction of the atria and then the sound caused by contraction of the ventricles.
The presence of both III and IV sounds at the same time is usually combined with pronounced tachycardia, therefore both additional tones merge into one sound, creating mesodiastolic "gallop rhythm".
Mitral valve opening tone is a characteristic sign of stenosis of the left atrioventricular orifice. It occurs immediately after the second sound, is best heard on the left side during exhalation and is perceived as a short, abrupt sound, reminiscent of a click. In contrast to bifurcation, the opening tone of the mitral valve is heard at the apex of the heart, and not at the base, and is combined with a melody characteristic of mitral stenosis (flapping 1st tone, diastolic murmur), forming a peculiar three-part rhythm - the “quail rhythm”. The occurrence of a “mitral click” is explained by the tension of the mitral valve leaflets fused along the commissures when they protrude into the cavity of the left ventricle during the opening of the valves in diastole.
In patients with constrictive pericarditis, after the second sound, a loud protodiastolic extratone at the apex, the so-called pericardial tone. Unlike the mitral click, it is not combined with an increased first sound.
Systolic extraton at the apex is most often associated with mitral valve prolapse. It is a sharp, loud, short sound.
Duplication and splitting of tones.
Heart sounds, although they consist of individual components, are perceived as a single sound due to their simultaneous and synchronous occurrence. If this synchrony is disrupted, the tone is perceived as two separate sounds. In the case when the pause between two sounds is barely distinguishable, they speak of splitting, if two parts of the tone are clearly heard - splitting tones.
Splitting of the first tone at the apex observed in healthy people at the end of inspiration or expiration and is associated with a change in blood flow to the heart.
Pathological splitting of the first tone observed when intraventricular conduction is disrupted as a result of delayed systole of one of the ventricles and, consequently, non-simultaneous closure of the atrioventricular valves. This is most often observed with bundle branch block, with a significant weakening of the contractile function of the myocardium or with pronounced hypertrophy of one of the ventricles.
Bifurcation of the second tone occurs when the aortic and pulmonary valves close at the same time. The duration of ventricular systole is determined by the volume of blood ejected and the pressure in the vessel where the blood enters. Thus, with a decrease in blood volume in the left ventricle and with low blood pressure in the aorta, the systole of the left ventricle will end sooner and the aortic valve leaflets will close earlier than the pulmonary valve leaflets. Therefore, bifurcation of the second tone can be observed when the blood supply to one of the ventricles in healthy people decreases or increases during one of the phases of breathing (end of inhalation or exhalation).
In pathology bifurcation of the second sound in the aorta associated with increased pressure in the systemic circulation (hypertension).
Bifurcation of the second tone on the pulmonary trunk associated with increased pressure in the pulmonary circulation (mitral stenosis, chronic lung diseases, stenosis of the pulmonary trunk), pathognomonic for atrial septal defect.
Heart murmurs- Murmurs are divided into intracardiac and extracardiac. They are complex, rich in overtones, longer sounds, heard in pauses between tones or merging with them. differ in their acoustic properties, timbre, and listening phase. Noises heard in the interval between tones I and II are called systolic, after the second tone - diastolic. The group of noises that occur with heart defects, as well as with myocardial damage, are called organic. Murmurs caused by other reasons and not combined with changes in tones, dilation of the heart chambers, or signs of heart failure are called functional. Extracardiac murmurs are included in a separate group.
Having identified a murmur during auscultation of the heart at standard points, it is necessary to determine:
The phase of the cardiac cycle in which it is heard;
Duration of the murmur (short, long) and what part of the cardiac cycle phase it occupies (protodiastolic, presystolic, pandiastolic, early systolic, etc.);
Timbre of noise (blowing, scraping, etc.);
The point of maximum noise volume and the direction of its conduction (left axillary fossa, carotid arteries, Botkin-Erb point);
Variability of noise depending on the phases of breathing and body position.
Following these rules often allows one to differentiate organic noises from functional ones.
Systolic organic murmurs occur with atrioventricular valve insufficiency, stenosis of the aorta and pulmonary trunk.
Systolic murmur at the apex heard with mitral valve insufficiency. The mechanism of its occurrence is as follows: during systole, the valves, deformed due to scar changes, do not completely block the hole, blood returns from the ventricles to the atrium through a narrow gap, and a vortex occurs - the noise of regurgitation. The noise is loud, rough, prolonged, has a decreasing character, is combined with a weakened 1st tone, and the 3rd tone is often detected. It intensifies in the position on the left side when holding your breath while exhaling, after physical activity, and radiates to the left axillary fossa.
Systolic murmur on the aorta heard when:
1) stenosis of the aortic mouth - ejection noise. This noise is usually loud, low-pitched, continuous, and extends to the carotid artery.
2) in elderly people, a systolic murmur may be heard on the aorta associated with atherosclerotic changes in the aortic valves.
Organic systolic murmur over the pulmonary trunk rarely heard. Its causes may be: stenosis of the mouth of the pulmonary trunk, atrial septal defect (soft, short-lived murmur), patent ductus arteriosus (systole-diastolic murmur, the systolic component of which is rough, loud, extends to the entire precordial region, neck vessels and into the axillary fossa) .
Systolic murmur due to tricuspid valve insufficiency is heard at the xiphoid process, has a decreasing character, is not always combined with a weakened first tone, is carried out on both sides of the sternum, and intensifies with inspiration (Rivero-Corvallo symptom).
The loudest and roughest systolic murmur is heard with a ventricular septal defect (Tolochinov-Roger disease). The epicenter of the sound is at the left edge of the sternum in the III-IV intercostal space, is better heard in the supine position, spreads to the left axillary fossa, interscapular space.
Diastolic murmurs- heard with narrowing of the atrioventricular orifices, insufficiency of the aortic and pulmonary valves.
Diastolic murmur over the apex of the heart heard with mitral orifice stenosis. In this case, blood enters diastole from the atria into the ventricles through a narrowed opening - a turbulence occurs, which is heard as noise. It is heard at the beginning of diastole (decreasing proto-diastolic), or at the end of it (increasing presystolic), and with severe mitral stenosis it becomes pan-diastolic. Usually heard in a limited area, better detected in a position on the left side, combined with the “quail rhythm”.
Diastolic murmur due to aortic valve insufficiency usually soft, decreasing, best heard at the Botkin-Erb point, in a standing position with the torso tilted forward or lying on the right side, combined with a weakened II tone. In this case, in diastole, the blood returns back through the loosely closed valve flaps from the aorta to the left ventricle - a vortex occurs, i.e. a noise that is loud at first and then gradually becomes less pronounced (decrescendo form).
Diastolic murmurs over the pulmonary trunk and at the xiphoid process are rarely heard and are associated with stenosis of the right atrioventricular orifice and pulmonary valve insufficiency, respectively.
Sometimes murmurs are heard over the entire area of the heart in one phase of cardiac activity, which makes diagnosis difficult. In this case, it is recommended:
1) listen to noise irradiation points, as mentioned above;
2) auscultation can be performed by moving the stethoscope along the line connecting the two points of listening to noise, from one valve to the other. A weakening or increasing volume of noise as you approach the second valve indicates damage to one valve. Above the valve, where it is heard weaker, the noise is wired. When, when moving the stethoscope, the noise first weakens and then intensifies again, one should think about damage to two valves.
Functional noise- are not associated with damage to the valves, valve orifices, or heart muscle. The following functional noises are distinguished:
Express;
Anemic;
Dystonic.
The difference between functional noise and organic noise:
More often these are systolic murmurs, not associated with the first sound;
They are heard in a limited area and do not radiate to other areas;
The sound is quiet, short, blowing, soft, with the exception of noises associated with dysfunction of the papillary muscles;
Labile, i.e. can change timbre, duration, arise or, conversely, disappear under the influence of various factors, changes in body position;
Not always accompanied by a change in the basic tones, the appearance of additional tones, expansion of the boundaries of the heart, signs of circulatory failure, and are not accompanied by “cat purring”;
Low amplitude, low frequency;
Reduce or disappear during treatment.
Functional systolic murmurs are most characteristic of childhood and adolescence. They are due to the following reasons:
Incomplete correspondence of the rates of development of various cardiac structures;
Dysfunction of papillary muscles;
Abnormal development of chords.
Systolic functional murmurs:
Relative insufficiency of the mitral valves. Occurs with severe dilatation of the left ventricle with expansion of the fibrous ring of the valves (dilated myocardiopathy, aortic defects, hypertension). Unlike the noise during a defect, this noise is softer, shorter lasting, and does not radiate.
Muscle noise occurs when the heart muscle is damaged (myocarditis, myocardiosclerosis, myocardial infarction) and is heard at the apex. The mechanism of its occurrence: non-simultaneous contraction of muscle fibers occurs, while the muscle component of the first tone increases in duration and creates the impression of noise.
Anemic noise. With anemia of various etiologies, blood thinning and blood flow speed accelerate. In this condition, the systolic murmur is heard over the entire region of the heart, but is better heard on the vessels, aorta and pulmonary trunk, where blood turbulence occurs, and intensifies when the patient moves from a horizontal to a vertical position, after physical exertion.
Diastolic functional murmurs:
Flint noise- functional diastolic murmur heard at the apex of the heart in patients with aortic valve insufficiency. With this defect, blood returning from the aorta to the left ventricle lifts the mitral valve leaflet, thereby creating a relative stenosis of the left atrioventricular orifice. At this time, the blood, when passing from the left atrium to the ventricle through a narrowed opening, swirls creating a functional noise that is heard in the diastole phase at the apex of the heart.
Graham-Still noise associated with expansion of the mouth of the pulmonary artery and stretching of its valve ring. This noise of relative pulmonary valve insufficiency is sometimes detected in patients with severe hypertension of the pulmonary circulation and is heard as a soft diastolic murmur in the second intercostal space on the left.
Coombs noise: Early diastolic murmur heard in the zone of absolute cardiac dullness near the apex. The mechanism of its occurrence is as follows: an increase in the speed of blood flow from the atrium to the left ventricle, with a decreased tone of the latter (the blood seems to freely “fall” into the cavity of the ventricle without encountering resistance).
Normally, heart sounds give the acoustic impression of a single short sound. In pathology, conditions are created for repeated multiple oscillations - for the emergence of noises that are perceived as sounds of a varied timbre. The main mechanism for the formation of noise is the passage of blood through a narrowed opening. An increase in blood flow speed contributes to the formation of noise; the blood flow speed depends on increased excitability and increased activity of the heart. The narrower the hole through which the blood passes, the stronger the noise, but with very strong narrowing, when the blood flow decreases sharply, the noise sometimes disappears. The noise intensifies as the contraction force increases and weakens as it decreases. Also, the acceleration of blood flow is associated with a decrease in blood viscosity (anemia). Types of noise Noises are divided into organic and functional. Organic noises are associated with pathological changes in the heart (valve apparatus changes: leaflets, tendon threads, capillary muscles), the size of the holes changes. The cause may be stenosis of the opening, which impedes the flow of blood to the next section; valve insufficiency, when the valve apparatus cannot completely close the hole to prevent the backflow of blood. Organic murmurs occur more often with valve defects and congenital heart defects. Functional noises are observed mainly in anemia, neuroses, infectious diseases, and thyrotoxicosis. The cause of the noise is the acceleration of blood flow (anemia, nervous excitement, thyrotoxicosis) or insufficient innervation or nutrition of the muscle fibers or capillary muscles of the heart, as a result of which the valve is not able to tightly close the corresponding hole. Functional murmurs differ from organic ones in their localization (determined on the pulmonary artery, apex of the heart); they are shorter in duration; depend on the psycho-emotional state and physical activity; as a rule, they intensify in a horizontal position; when listening, they are tender, blowing, weak; they are transient in nature (they decrease as the condition improves). Based on the time the noise appears during systole or diastole, systolic and diastolic murmurs are distinguished. Systolic murmur is heard in the vast majority of functional murmurs; with mitral and tricuspid valve insufficiency; with stenosis of the aortic mouth; with stenosis of the pulmonary artery; with atherosclerotic lesions of the walls and aortic aneurysm; with an open interventricular foramen. Systolic murmur appears in the first minor pause and corresponds to ventricular systole; the first sound is often absent, but may persist. Diastolic murmur is heard with aortic valve insufficiency; pulmonary valve insufficiency; non-closure of the ductus botallus; with stenosis of the left atrioventricular orifice. Diastolic murmur appears in the second major pause and corresponds to ventricular diastole.
The noise that occurs at the very beginning of diastole is called protodiastolic(occurs with valve insufficiency; left atrioventricular stenosis; patent ductus botallus). Presystolic murmur is a murmur that occurs at the end of diastole (mitral stenosis). A murmur that occupies only the middle of diastole is called mesodiastolic. Diastolic murmur detected by auscultation on the aorta makes it possible to confidently speak about aortic valve insufficiency; presystolic murmur at the apex practically makes it possible to diagnose stenosis of the left atrioventricular orifice. Unlike diastolic murmur, systolic murmur has less important diagnostic value. So, for example, when listening to a systolic murmur at the apex, it can be explained by organic or muscle failure, as well as functional changes. Noises are heard in the classic places where tones are detected, as well as at some distance from them, along the path of the blood flow. The sound of aortic valve insufficiency is carried to the ventricle, to the left and down, and is better heard along the left edge of the sternum at the level of the third costal cartilage (64). With stenosis of the aortic mouth, the noise passes into the carotid artery, into the jugular fossa. In rheumatic endocarditis, in the initial stages of damage to the aortic valves, a murmur is detected at the left edge of the sternum in the third or fourth intercostal space. In case of mitral valve insufficiency, the noise is carried up to the second intercostal space or to the left to the armpit. Presystolic murmur with mitral stenosis is detected at the apex of the heart, occupying a very small space. The strength of the noise depends on the speed of blood flow created by the heart itself and on the narrowness of the opening. In some cases - with a very large or very small narrowing of the hole - the noise becomes very weak and inaudible. Diagnostically, variability in murmur intensity over time is valuable. So, with endocarditis, new deposits or destruction of the valve can increase the noise, which is a bad sign. In other cases, the increase in noise depends on the increase in the strength of the heart muscle and is an indicator of improvement. Clinic and laboratory data allow us to understand changes in noise over time. The nature of the noises is soft, blowing and rough, sawing, scraping, etc. Organic noises, as a rule, are rough. Soft, blowing - both organic and functional. The height and nature of the noise are rarely of practical importance.
Systolic murmur:
This is a noise that is heard after the 1st tone and appears due to the fact that during contraction of the ventricles, blood is expelled from it through a narrowed opening. The noise occurs simultaneously with the 1st tone or shortly after it. With a sharp weakening of the 1st tone or in those cases when a rough, as if systolic murmur overlaps the 1st tone, its identification is helped by the sign that the murmur coincides, like the 1st tone, with the apical impulse\if it is palpated\ and the pulse in the carotid arteries.
Most of the systolic murmurs are heard over the heart, especially over the pulmonary artery and aorta, and are a consequence of anemia, tachycardia\with hypothyroidism, high temperature\these are random accidental noises. A diagnosis of the heart cannot be made on the basis of systolic murmur alone. It is important to differentiate accidental ones murmurs from pathological ones. The first ones are usually softer and are heard at the base of the heart and partly over the entire surface of the heart. systolic murmur at the apex conducted in the direction of the left axillary cavity and in the direction of the place where the aortic valves are heard - a sign of blood regurgitation through the left venous opening - the cause of insufficiency 2-leaf valve, which could be caused by endocarditis, dilatation of the left ventricle, cardiosclerosis, aortic insufficiency. with true insufficiency of the 2-leaf valve, there is a weakening of the 1st tone, systolic murmur, expansion of the left ventricle and left ventricle, displacement of the apical impulse down and out and an intensified 2nd tone above the pulmonary artery. More often, the systolic murmur is blowing loud begins with a weakened 1st tone and continues throughout the entire systole.
A noise heard to the left of the sternum in the 3rd-4th intercostal space occurs during a heart attack and is a sign of perforation of the septum. A similar noise is observed with a congenital defect of the interventricular septum\murmur of the erysipelas\
A murmur heard above the aorta and conducted in the direction of the shoulder of the occipital neck is characteristic of aortic stenosis. If there is significant stenosis, the 2nd sound may be absent or audible, but it will be delayed. For this lesion, there is always a pause between the end of the noise and the 2nd tone.
Coarctation of the aorta also causes a systolic/ejection murmur, but in late systole it is best heard on the back of the scapula.
Systolic murmur may also be caused by pulmonary artery stenosis; in this case, it is heard before the appearance of the 2nd sound
When the RV is overloaded, a relative stenosis of the pulmonary artery occurs and it is heard in the 3rd intercostal space along the left edge of the sternum. A systolic murmur above the site where the pulmonary artery is heard is not a pathological sign, especially at a young age.
Systolic murmur along the right edge of the sternum can occur with insufficiency of the 3-leaf valve. With its insufficiency, a positive venous pulse and a large pulsating liver are observed.
Tetralogy of Fallot is characterized by an intense systolic murmur heard over almost the entire surface of the heart, while the 2nd tone is very weakened or inaudible. This disease is congenital; its symptoms are cyanosis, shoe-shaped heart\clog\erythrocytosis, drum fingers, developmental delay.
Systylic murmur of a musical nature occurs with sclerotic narrowing of the aortic orifice or with sclerotic changes in the mitral valve. Less often with dissecting aortic aneurysm. A systolic noise heard over the vessels is characteristic of an aortic aneurysm. atherosclerotic narrowing and aortitis
Acquired and congenital heart defects. Clinical and physical landmarks.
Acquired defects:
Stenosis of the mitral (left ventricle and left atrium) orifice: signs pulmonary hypertension(up to pulmonary edema), right ventricular hypertrophy. Palpation - “cat purring” (diastolic trembling), pulse on the left hand > pulse on the right. Auscultation – quail rhythm (flapping 1st tone + click of the mitral valve opening + increased 2nd tone), diastolic murmur at the mitral valve point, diastolic murmur at the pulmonary artery point.
Mitral valve insufficiency: signs of pulmonary hypertension, right ventricular hypertrophy. Auscultation – weakened 1st sound, possible splitting of the 2nd tone, pathological 3rd tone, accent of the 2nd tone over the pulmonary trunk. Systolic murmur at the apex.
Aortic stenosis: signs of hypertrophy of the left ventricle, left atrium, stagnation in the pulmonary circle (orthopnea, pulmonary edema, cardiac asthma). Auscultation – weakened 2nd sound, splitting of the 2nd tone, “scraping” systolic murmur, click of the jet hitting the aortic wall.
Aortic valve insufficiency: physically – “dance of the carotid”, Mr. de Mussy, capillary pulse, pulsation of the pupils and soft palate. Auscultation - cannon tone (Traube) on the femoral artery, systolic murmur on the femoral artery, weakened or enhanced (can be either way) 1st tone, diastolic murmur, mid-diastolic (presystolic) Austin-Flint murmur.
Congenital defects:
VSD: 3 degrees: 4-5 mm, 6-20 mm, >20 mm. Signs: developmental delay, congestion in the ICB, frequent lung infections, shortness of breath, liver enlargement, edema (usually of the limbs), orthopnea. Auscultation - systolic murmur to the left of the sternum.
ASD: The discharge of blood is always from left to right. Auscultation – splitting of the 2nd tone, systolic murmur on the pulmonary artery.
Botall's duct(m/n pulmonary artery and aorta): systolic and diastolic “machine” murmur.
Coartation of the aorta: hypertension, better development of the torso, blood pressure in the legs<АД на руках.
14. Broncho-obstructive syndrome is a collective term that includes a symptom complex of specifically defined clinical manifestations of bronchial obstruction, which is based on narrowing or occlusion of the airways.
From a practical point of view, depending on the etiological pathogenetic mechanisms, there are 4 variants of biofeedback:
infectious, developing as a result of viral and (or) bacterial inflammation in the bronchi and bronchioles;
allergic, developing as a result of spasm and allergic inflammation of bronchial structures with a predominance of spastic phenomena over inflammatory ones;
obstructive, observed during aspiration of a foreign body, with compression of the bronchi;
hemodynamic, which occurs in heart failure of the left ventricular type.
According to the course of biofeedback, it can be acute, protracted, recurrent and continuously recurrent (in the case of bronchopulmonary dysplasia, bronchiolitis obletus, etc.).
According to the severity of obstruction, one can distinguish: mild degree of obstruction (1st degree), moderate (2nd degree), severe (3rd degree).
In the genesis of bronchial obstruction in acute respiratory infections, swelling of the mucous membrane, inflammatory infiltration, and hypersecretion are of primary importance. To a lesser extent, the mechanism of bronchospasm is expressed, which is caused either by increased sensitivity of the interoreceptors of the cholinergic link of the VNS (primary or secondary hyperactivity), or by blockade of B2-adrenergic receptors. The viruses that most often cause obstructive syndrome include the RS virus (about 50%), then the parainfluenza virus, mycoplasma pneumoniae, and less commonly, influenza viruses and adenovirus.
BOS of infectious origin most often occurs in obstructive bronchitis and bronchiolitis.
Obstruction in allergic diseases is caused mainly by spasm of small bronchi and bronchioles (tonic type) and to a lesser extent by hypersecretion and edema. Significant difficulties are presented by the differential diagnosis between asthmatic bronchitis and obstructive bronchitis of infectious origin. In favor of asthmatic bronchitis is evidenced by a family history of allergic diseases, a burdened personal allergy history (skin manifestations of allergies, “minor” forms of respiratory allergosis - allergic rhinitis, laryngitis, tracheitis, bronchitis, intestinal allergosis), the presence of a connection with the occurrence of the disease with a causally significant allergen and the absence of such a connection with the infection, a positive elimination effect, recurrence of attacks, their uniformity. The wedge picture is characterized by the following signs: absence of intoxication phenomena, remote wheezing or “sawing” nature of breathing, expiratory shortness of breath with the participation of auxiliary muscles, in the lungs there are predominantly dry wheezing and a few wet ones, the number of which increases after relief of bronchospasm. An attack usually occurs on the first day of the disease and is eliminated in a short time: within one to three days. In favor of asthmatic bronchitis, the positive effect of the administration of bronchospasmolytics (adrenaline, aminophylline, berotec, etc.) is also evidenced. The cardinal sign of bronchial asthma is an attack of suffocation.
Not every person has heard of such a concept as systolic sounds. It is worth saying that this condition may indicate the presence of serious pathologies in the human body. A systolic murmur in the heart indicates that there is a malfunction in the body.
What is he talking about?
If a patient experiences sounds inside the body, this means that the process of blood flow in the heart vessels is disrupted. There is a widespread belief that systolic murmur occurs in adults.
This means that a pathological process is occurring in the human body, which indicates some kind of illness. In this case, it is necessary to urgently undergo a cardiac examination.
Systolic murmur is defined as its presence between the second heart sound and the first. The sound is recorded on the heart valves or blood flow.
Division of noise into types
There is a certain gradation of separation of these pathological processes:
- Functional systolic murmur. It refers to innocent manifestation. Does not pose a danger to the human body.
- Systolic murmur of organic type. Such a noise character indicates the presence of a pathological process in the body.
An innocent type of noise may indicate that there are other processes in the human body that are not related to heart disease. They are mild in nature, do not last long, and have a weakly expressed intensity. If a person reduces physical activity, the noise will disappear. Data may vary depending on the patient's posture.

Noise effects of a systolic nature arise due to septal and valvular disorders. Namely, in the human heart there is dysfunction of the partitions between the ventricles and atria. They differ in the nature of their sound. They are hard, tough and stable. A rough systolic murmur is present and its long duration is recorded.
These sound effects extend beyond the boundaries of the heart and are reflected in the axillary and interscapular areas. If a person has subjected his body to exercise, then sound deviations persist after completion. Noises become louder during physical activity. The organic sound effects that are present in the heart are independent of body position. They can be heard equally well in any position of the patient.
Acoustic value
Heart sound effects have different acoustic meanings:
- Systolic murmurs of early manifestation.
- Pansystolic murmurs. They also have the name holosystolic.
- Mid-late murmurs.
- Systolic murmur at all points.
What factors influence the occurrence of noise?
What are the causes of systolic murmur? There are several main ones. These include:
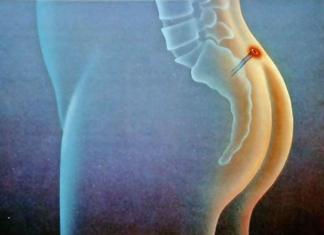
- Aortic stenosis. It can be either congenital or acquired. This disease occurs due to narrowing of the aorta. With this pathology, the walls of the valve become fused. This position makes it difficult for blood to flow inside the heart. Aortic stenosis can be considered the most common heart defect in adults. The consequence of this pathology can be aortic insufficiency, as well as mitral disease. The aortic system is designed in such a way that calcification is produced. In this regard, the pathological process intensifies. It is also worth mentioning that with aortic stenosis, the load on the left ventricle increases. At the same time, the brain and heart experience insufficient blood supply.
- Aortic insufficiency. This pathology also contributes to the occurrence of systolic murmur. With this pathological process, the aortic valve does not close completely. Infectious endocarditis causes aortic insufficiency. The impetus for the development of this disease is rheumatism. Lupus erythematosus, syphilis and atherosclerosis can also provoke aortic insufficiency. But injuries and congenital defects rarely lead to this disease. A systolic murmur in the aorta indicates that the valve has aortic insufficiency. The reason for this may be expansion of the ring or aorta.
- Washing of the acute course is also the reason why systolic murmurs appear in the heart. This pathology is associated with the rapid movement of liquids and gases in the hollow regions of the heart during their contraction. They are moving in the opposite direction. As a rule, this diagnosis is made when the functioning of the dividing partitions is impaired.
- Stenosis. This pathological process is also the cause of systolic murmurs. In this case, a narrowing of the right ventricle, namely its tract, is diagnosed. This pathological process occurs in 10% of cases of murmurs. In this situation, they are accompanied by systolic tremors. The vessels of the neck are especially susceptible to irradiation.
- Tricuspid valve stenosis. With this pathology, the tricuspid valve narrows. As a rule, rheumatic fever leads to this disease. Patients experience symptoms such as cold skin, fatigue, and discomfort in the neck and abdomen.
Why does noise appear in children?
Why might a child have a heart murmur? There are many reasons. The most common ones will be listed below. So, heart murmurs may occur in a child due to the following pathologies:


Congenital heart defects in children
It is worth saying a few words about newborn babies. Immediately after birth, a complete examination of the body is carried out. This includes listening to the heart rate. This is done in order to exclude or detect any pathological processes in the body.
With such an examination, there is a possibility of detecting any noise. But they shouldn't always be a cause for concern. This is due to the fact that noises are quite common in newborn babies. The fact is that the child’s body adapts to the external environment. The cardiac system is reconfigured, so different noises are possible. Further examination through methods such as x-ray and electrocardiogram will show whether any abnormality is present or not.
The presence of congenital noises in the baby’s body is determined during the first three years of life. Murmurs in newborn babies may indicate that the heart was not fully formed during development before birth for various reasons. In this regard, after birth the baby develops noises. They talk about congenital defects of the cardiac system. In cases where pathologies have a high risk for the child’s health, doctors decide on a surgical method of treating a particular pathology.
Noise features: systolic murmur at the apex of the heart and in other parts of it
It is worth knowing that the characteristics of noise may vary depending on their location. For example, there is a systolic murmur at the aortic apex.
- Mitral valve pathology and associated acute insufficiency. In this position, the noise is short-lived. Its manifestation occurs early. If this type of noise is detected, then the patient is diagnosed with the following pathologies: hypokinesis, chord rupture, bacterial endocarditis, etc.
- Systolic murmur on the left sternal border.
- Chronic mitral valve insufficiency. This type of noise is characterized by the fact that they occupy the entire duration of ventricular contraction. The size of the valve defect is proportional to the volume of blood returned and the nature of the murmur. This noise is better heard if a person is in a horizontal position. As the heart defect progresses, the patient experiences vibration in the chest. There is also a systolic murmur at the base of the heart. Vibration is felt during systole.
- Mitral insufficiency of a relative nature. This pathological process is treatable with proper treatment and compliance with recommendations.
- Systolic murmur in anemia.
- Pathological disorders of the papillary muscles. This pathology refers to myocardial infarction, as well as ischemic disorders in the heart. This type of systolic murmur is variable. It is diagnosed at the end of systole or in the middle. There is a short systolic murmur.
The appearance of heart murmurs during pregnancy in women
When a woman is pregnant, processes such as systolic murmurs cannot be ruled out in her heart. The most common cause of their occurrence is the load on the girl’s body. Typically, heart murmurs appear in the third trimester.

If they are detected in a woman, the patient is placed under more careful monitoring. At the medical institution where she is registered, her blood pressure is constantly measured, her kidney function is checked, and other measures are taken to monitor her condition. If a woman is constantly under observation and follows all the recommendations that doctors give her, then bearing a child will be in a good mood without any consequences.
How are diagnostic procedures carried out to detect heart murmurs?
First of all, doctors are faced with the task of determining whether there is a heart murmur or not. The patient undergoes an examination such as auscultation. During it, the person must first be in a horizontal position and then in a vertical position. Listening is also performed after physical exercise in a position on the left side while inhaling and exhaling. These measures are necessary to accurately determine noise. Since they can have a different nature of occurrence, an important point is their accurate diagnosis.
For example, in case of pathology of the mitral valve, it is necessary to listen to the apex of the heart. But in case of tricuspid valve defects, it is better to examine the lower edge of the sternum.
An important point in this matter is the exclusion of other noises that may be present in the human body. For example, with a disease such as pericarditis, murmurs may also occur.
Diagnostic options
In order to diagnose noise effects in the human body, special technological means are used, namely: PCG, ECG, radiography, echocardiography. X-ray of the heart is done in three projections.

There are patients for whom the above methods may be contraindicated, since they have other pathological processes in the body. In this case, the person is prescribed invasive examination methods. These include probing and contrast methods.
Samples
Also, to accurately diagnose the patient’s condition, namely, to measure the intensity of noise, various tests are used. The following methods are used:
- Loading the patient with physical exercises. Isometric, isotonic, carpal dynamometry.
- Listen to the patient's breathing. It is determined whether the sounds become louder when the patient exhales.
- Extrasystole.
- Changing the posture of the person being examined. Namely, raising the legs when a person is standing, squatting, etc.
- Holding your breath. This examination is called the Valsalva maneuver.
It is worth saying that it is necessary to carry out timely diagnostics to identify murmurs in a person’s heart. An important point is to establish the cause of their occurrence. It should be remembered that systolic murmur may mean that a serious pathological process is occurring in the human body. In this case, identifying the type of noise at an early stage will help to take all necessary measures to treat the patient. However, they also may not have any serious deviations behind them and will pass after a certain time.

It is necessary for the doctor to carefully diagnose the noise and determine the cause of its appearance in the body. It is also worth remembering that they accompany a person at different age periods. You should not take these manifestations of the body lightly. It is necessary to complete diagnostic activities. For example, if a noise is detected in a woman who is pregnant, then monitoring her condition is mandatory.
Conclusion
It is recommended to check the functioning of the heart even if a person has no complaints about the functioning of this organ. Systolic murmurs may be detected incidentally. Diagnosing the body allows you to identify any pathological changes at an early stage and take the necessary treatment measures.