Treatment of acute renal failure must begin with the treatment of the underlying disease that caused it.
To assess the degree of fluid retention in the patient's body, daily weighing is desirable. For a more accurate determination of the degree of hydration, volume infusion therapy and indications for it, it is necessary to install a catheter in central vein. It should also take into account the daily diuresis, as well as the patient's blood pressure.
In case of prerenal acute renal failure, it is necessary to restore the BCC as soon as possible and normalize blood pressure.
For the treatment of renal acute renal failure caused by various substances of medicinal and non-drug nature, as well as some diseases, it is necessary to start detoxification therapy as early as possible. It is desirable to take into account the molecular weight of the toxins that caused acute renal failure, and the clearance capabilities of the efferent therapy method used (plasmapheresis, hemosorption, hemodiafiltration or hemodialysis), the possibility of the earliest administration of the antidote.
In postrenal acute renal failure, immediate drainage of the urinary tract is necessary to restore adequate urine flow. When choosing the tactics of surgical intervention on the kidney in conditions of acute renal failure, even before the operation, information about the sufficient function of the contralateral kidney is necessary. Patients with a single kidney are not so rare. During the stage of polyuria, which usually develops after drainage, it is necessary to control the fluid balance in the patient's body and the electrolyte composition of the blood. The polyuric stage of acute renal failure may present with hypokalemia.
Medical treatment of acute renal failure
With an intact passage through the gastrointestinal tract, adequate enteral nutrition is necessary. If it is impossible, the need for proteins, fats, carbohydrates, vitamins and minerals is satisfied with the help of intravenous nutrition. Given the severity of the violation glomerular filtration protein intake is limited to 20-25 g per day. The required caloric intake should be at least 1500 kcal / day. The amount of fluid required by the patient before the development of the polyuric stage is determined based on the volume of diuresis for the previous day and an additional 500 ml.
The combination of acute renal failure and urosepsis causes the greatest difficulty in treatment. The combination of two types of uremic and purulent intoxication at once significantly complicates the treatment, and also significantly worsens the prognosis for life and recovery. In the treatment of these patients, it is necessary to use efferent methods of detoxification (hemodiafiltration, plasmapheresis, indirect electrochemical blood oxidation), selection antibacterial drugs according to the results bacteriological analysis blood and urine, as well as their dosing, taking into account the actual glomerular filtration.
Treatment of a patient with hemodialysis (or modified hemodialysis) cannot serve as a contraindication to surgical treatment of diseases or complications that led to acute renal failure. Modern possibilities of monitoring the blood coagulation system and its drug correction allow avoiding the risk of bleeding during operations and in postoperative period. For efferent therapy, it is desirable to use short-acting anticoagulants, for example, sodium heparin, the excess of which can be neutralized by the end of treatment with an antidote - protamine sulfate; sodium citrate can also be used as a coagulant. To control the blood coagulation system, the study of activated partial thromboplastin time and the determination of the amount of fibrinogen in the blood are usually used. The method for determining blood clotting time is not always accurate.
Treatment of acute renal failure even before the development of the polyuric stage requires the appointment of loop diuretics, such as furosemide up to 200-300 mg per day fractionally.
Anabolic steroids are prescribed to compensate for catabolism processes.
Indicated for hyperkalemia intravenous administration 400 ml of 5% glucose solution with 8 units of insulin, as well as 10-30 ml of 10% calcium gluconate solution. If hyperkalemia cannot be corrected conservative methods, then the patient is indicated for emergency hemodialysis.
Surgical treatment of acute renal failure
To replace kidney function during the period of oliguria, you can use any method of blood purification:
- hemodialysis;
- peritoneal dialysis;
- hemofiltration;
- hemodiafiltration;
- low flow hemodiafiltration.
With multiple organ failure, it is better to start with low-flow hemodiafiltration.
Treatment of acute renal failure: hemodialysis
Indications for hemodialysis or its modification in chronic and acute renal failure are different. In the treatment of acute renal failure, the frequency, duration of the procedure, dialysis load, filtration value and composition of the dialysate are selected individually at the time of the examination, before each treatment session. Treatment with hemodialysis is continued, preventing an increase in the urea content in the blood above 30 mmol / l. With the resolution of acute renal failure, the blood creatinine concentration begins to decrease earlier than the blood urea concentration, which is regarded as a positive prognostic sign.
Emergency indications for hemodialysis (and its modifications):
- "uncontrolled" hyperkalemia;
- severe hyperhydration;
- hyperhydration of lung tissue;
- severe uremic toxicity.
Planned indications for hemodialysis:
- the content of urea in the blood is more than 30 mmol / l and / or the concentration of creatinine in excess of 0.5 mmol / l;
- pronounced Clinical signs uremic intoxication (such as uremic encephalopathy, uremic gastritis, enterocolitis, gastroenterocolitis);
- hyperhydration;
- severe acidosis;
- hyponatremia;
- a rapid (within a few days) increase in the content of uremic toxins in the blood (daily increase in urea exceeding 7 mmol / l, and creatinine - 0.2-0.3 mmol / l) and / or a decrease in diuresis
With the onset of the stage of polyuria, the need for hemodialysis treatment disappears.
Possible contraindications to efferent therapy:
- afibrinogenemic bleeding;
- unreliable surgical hemostasis;
- parenchymal bleeding.
As a vascular access for dialysis treatment, a two-way catheter is used, installed in one of the central veins (subclavian, jugular or femoral).
Quick page navigation
The main task that we must solve is to simply and intelligibly tell about the mechanisms of development, symptoms and principles of treatment of both acute and chronic renal failure in women and men. The difficulty lies in the fact that with the undoubted similarity of processes, there is a significant difference between acute and chronic renal failure.
There are no differences between female kidney failure and male kidney failure. The kidneys, as an organ, do not have gender differences in structure and function. Therefore, women may special reasons its occurrence, which men do not have.
For example, during pregnancy, the uterus “squeezes” the ureter, an expansion of the pyelocaliceal system of the kidneys occurs, and develops. But pregnancy is a short period, and, as a rule, kidney failure simply does not have time to develop.
Very roughly, but true, a chronic condition in diseases can be compared with a slightly forgetful, but quite “adequate” patient with cerebral atherosclerosis, and acute renal failure can be compared with a stroke or stroke. In this case, everything here will be different - the treatment is calculated by the hour, all the principles and protocols for managing the patient will be special. And, it would seem, only chronic disorders turned into acute ones.
The difficulty lies in the fact that acute renal failure, or acute renal failure, is a condition that may not be related to the kidneys at all, and occur against the background of their complete health.
Why this condition arises and develops, we will explain below, but first we should talk very briefly about how the normal kidney works, so that the course of further presentation is clear.
A bit of physiology
Get used to the idea that urine is the former blood, its liquid part, and former blood recently. The formation of urine occurs in several stages:
- In the cortical layer of the kidney, in the glomeruli of nephrons (this is the structural and functional unit of the kidney), there is a constant primary filtration of blood.
Its normal rate is 120 ml/min. But a person cannot afford the luxury of excreting primary urine, since its volume would be about 200 liters per day. According to losses, a person would have to replenish the same volume all the time.
It is clear that, apart from drinking and urinating, humanity would have no time for anything, and we would not have come out of the sea to land. Therefore, urine must be concentrated - in other parts of the nephron, urine is concentrated 100 times, and in this form it enters the ureter.
Of course, in addition to concentration, very important processes take place, for example, reabsorption or reabsorption of many important compounds from the primary filtrate into the blood, for example, glucose, which simply passed through the primary filter. The concentration of urine requires a large expenditure of energy.
Thus, the kidneys are organs that maintain homeostasis, that is, the constancy of the internal environment of the body. In addition to participating in water and salt metabolism, the kidneys decide the fate of hundreds of different compounds, and also participate in the production of various substances (for example, erythropoietins that stimulate hematopoiesis).
What we end up with is normal urine that excretes whatever it shouldn't and doesn't let "deficiency" in, like protein pass through. But in kidney failure, these mechanisms are disrupted, and the urine of a patient with kidney failure resembles a frontier where drug and smuggling channels are established, and unplanned penetrations occur. What is kidney failure?
Differences between acute and chronic renal failure
 AKI (acute renal failure) and CKD (chronic renal failure) is a violation of the homeostatic function of the kidneys. In the case of acute renal failure, it sometimes develops in a few hours or days, and in the case of chronic renal failure, it can progress for years.
AKI (acute renal failure) and CKD (chronic renal failure) is a violation of the homeostatic function of the kidneys. In the case of acute renal failure, it sometimes develops in a few hours or days, and in the case of chronic renal failure, it can progress for years.
- The most important difference between these conditions is the fact that in acute renal failure, the kidneys are most often “not to blame” - they are taken by surprise by an emergency situation, and they cannot cope with the function, simply, “like everyone else”, participating in a whole cascade of metabolic disorders.
Chronic renal failure is a condition in which it is the kidneys that are to blame, and a "test of reserves" occurs. With chronic renal failure, its slow development allows you to compensate, develop temporary measures, adapt, and as a result, maintain kidney function at a decent level for a long time, without a threat to life.
So, it is known that there are 2 million nephrons in the kidneys. Even if half die (which is tantamount to the loss of one kidney), then there may be no signs of illness. And only when only 30% of nephrons remain in the kidneys, and the filtration rate drops three times, to 40 ml / min, then clinical signs of CRF appear.
- A mortal threat to life occurs when 90% of nephrons die.
Acute kidney failure - what is it?

Acute renal failure syndrome occurs in one patient in 5000 cases. This is not much, given the spontaneous nature of the occurrence. But, on the other hand, in a large regional or regional center with a population of 1 million people, there will already be about 200 patients during the year, and this is a lot.
From the history of the issue, it can be established that in 90% of cases, acute renal failure occurred in the middle of the twentieth century, as a complication of criminal abortion. Currently, acute renal failure occurs in various fields of medicine, and is most often a manifestation of multiple organ failure syndrome. Distinguish:
- Prerenal acute renal failure (that is, prerenal) - 50%.
Prerenal acute renal failure occurs with completely intact kidney function. But arrhythmias, various shocks, embolism pulmonary artery and heart failure simply cannot provide "pressure supply" to the kidney system.
Also, acute renal failure develops with vasodilation (with allergic shock, or anaphylaxis, with sepsis). Of course, if a significant amount of fluid has disappeared from the body (bleeding, severe diarrhea), then this will also lead to an elementary lack of filtration volume.
- Renal (acute damage to nephrons);
According to statistics, almost all renal acute renal failure is caused by either ischemia or nephron intoxication. Almost always, with this violation, acute tubular necrosis occurs, that is, the “death” of the urine concentration apparatus. For example, this type of acute renal failure occurs when there is a massive influx of muscle breakdown products (myoglobin) into the blood during prolonged crush syndrome, or crash syndrome, shortly after improper removal of compression.
It is also caused by some drugs (antibiotics - aminoglycosides), NSAIDs, x-ray contrast agents, captopril.
In 1998, a case was described when, after a single injection of cefuroxime (an antibiotic from the cephalosporin group), a patient developed acute bilateral necrosis. As a result, she lived on hemodialysis for 1.5 years, and her condition improved only after a kidney transplant.
- Postrenal (postrenal, urinary outflow is disturbed) - 5%.
This type of acute renal failure is rare, and can occur in unconscious, elderly and mentally ill patients. Accompanied by anuria (less than 50 ml per day). The reason is stones, adenoma, cancer and others leading to obstruction at any level, from the urethra to the pelvis, obstruction of the passage of urine.
Symptoms of acute renal failure
OPN develops in stages. With a favorable outcome, these are: the initial, oliguric stage, the restoration of diuresis and recovery.
There are no specific symptoms of acute renal failure. The following general features can be distinguished:
- collapse, or low blood pressure;
- oliguria (reduced amount of urine);
- nausea, diarrhea, bloating, refusal to eat;
- anemia;
- hyperkalemia;
- the development of acidosis and "acidification" of the blood, the appearance of Kussmaul's noisy breathing.
The clinical presentation of ARF is very variable. So, hyperkalemia occurs with extensive burns, anemia - with severe hemolysis, convulsions and fever, sweating - with septic shock. Thus, acute renal failure proceeds under the guise of the cause that caused it.
Its main indicators will be the growth of blood urea against the background of a sharp decrease in the amount of urine.
Treatment of acute renal failure
It is known that various shocks (cardiogenic, burn, pain, infectious-toxic, anaphylactic) are the cause of acute renal failure in 90% of cases.
Therefore, the fight against shock allows and resolve acute renal failure. To do this, they replenish the volume of circulating blood, limit the intake of potassium, conduct blood transfusions, and provide a protein-free diet. For severe disorders, hemodialysis is used.
In infections and sepsis, dialysis is combined with hemosorption, UV blood. In blood diseases that lead to anemia, plasmapheresis is used.
The treatment of acute renal failure is an art, as doctors are constantly limited in their abilities. So, with an infectious-toxic shock that led to acute renal failure, you need to cope with the infection as soon as possible, but the use effective drugs limited, because renal function is reduced and the possibility of toxic damage to the glomeruli must be considered.
Forecast
As a rule, with isolated kidney failure, mortality does not exceed 10-15%, but it rapidly increases to 70% in old age, against the background of acute cardiac or liver failure, reaching up to 100% in the presence of "all deficiencies", or multiple organ failure.
In those who survive, kidney function is fully restored, according to various sources, in 30-40% of cases. If we talk about long-term complications, then most often there are pyelonephritis associated with stagnation of urine during acute renal failure.
Chronic renal failure - what is it?

Let us now turn to slowly emerging CRF, the outcome of which is a uremic coma, with the "death knell" of the uremic as a symptom immediately preceding the coma. This is the name given to the rough, screeching pericardial friction noise that occurs in patients in the terminal stage of CRF.
It arose because urea, which was formed as a result of protein breakdown, was not excreted by the kidneys and was deposited in the form of inorganic crystals throughout the body, including in the pericardial cavity.
Of course, at present, such symptoms, and especially those first detected, are practically non-existent - but chronic renal failure can lead to this. What causes CKD?
Causes of CRF
The main diseases leading to chronic renal failure affect the glomeruli of the kidneys, which filter the primary urine, and the tubules. The connective tissue of the kidneys, or interstitium, in which the nephrons are immersed, can also be affected.
CRF also causes rheumatic diseases that affect the connective tissue, metabolic diseases and congenital anomalies of the kidneys. Contributing their "contribution" vascular lesions and conditions occurring with obstruction of the urinary tract. Here are some of these diseases:
- glomerulonephritis, chronic pyelonephritis, interstitial nephritis;
- systemic scleroderma, hemorrhagic vasculitis;
- diabetes, amyloidosis;
- polycystic kidney disease, congenital hypoplasia;
- malignant renal hypertension, stenosis of the renal arteries;
The basis of the defeat of the nephron in chronic renal failure, regardless of the cause, is glomerulosclerosis. The glomerulus becomes empty and is replaced by connective tissue. Uremia occurs in the blood, that is, roughly speaking, "urination".
Circulating uremic toxins (urea, creatinine, parathyroid hormone, beta microglobulin) poison the body, accumulating in organs and tissues.
Symptoms of chronic renal failure
Symptoms of chronic renal failure in women and men are the same, and begin with disorders of water-salt metabolism.
There are four stages in the course of CKD:
1) Latent, which corresponds to the onset of water-salt disorders.
Everything starts on early stages HPN:
- Isosthenuria and hypostenuria. The kidneys cannot concentrate urine. Urine "holds out" only to a density of 1010-1012, and with hypostenuria, in general, up to 1008.
- Nocturia, or the predominance of nighttime urine volume over daytime. Healthy nephrons are overloaded and work the "night shift". This occurs, for example, because the spasm of the kidney vessels is eliminated at night;
- Polyuria. The amount of urine increases, compensating for the lack of "quality". In the terminal stage of renal failure, the amount of urine decreases to 600-800 ml per day, which is an indication for dialysis.
2) Compensated, in which the kidneys still cope and there is no oliguria.
All this leads to salt depletion - there is weakness, a decrease in pressure. But in some patients, sodium retention, on the contrary, causes an increase in blood pressure. Sleep is also disturbed, appetite decreases.
fatigue occurs, headache, pruritus, dizziness, depression. The body temperature drops, bleeding occurs. The delay of potassium and magnesium leads to muscle weakness, disruption of the heart, and drowsiness.
3) Intermittent (fluctuating) when periods of oliguria occur and the accumulation of ions in the plasma increases.
The most common are thirst, nausea, vomiting, bad taste in the mouth, stomatitis, and ammonia breath. The skin is pale, dry and flabby. There is a small tremor of the fingers.
At the advanced stage of chronic renal failure, anemia often occurs, since the kidneys produce a substance that affects the synthesis of red blood cells. Clinical picture reflects azotemia, that is, the accumulation of protein metabolism products in the body.
4) Terminal.
encephalopathy occurs. Memory is disturbed, insomnia occurs. Muscle weakness appears, it is difficult to climb stairs. Then there is excruciating skin itching, paresthesia, increased subcutaneous bleeding, nosebleeds appear.
In severe cases, due to water retention and "water poisoning", there is pulmonary edema, chronic heart failure, and myocardial dystrophy develops. Progresses ("crawling", numbness, pain), worsens, or the sense of smell and taste disappear.
The retina is affected, which can lead to complete blindness, stunning and uremic coma develop. Patients emit a strong smell of ammonia.
Treatment of chronic renal failure + diet
Since CRF is long-term, all measures must be taken already at the initial stages: this is a diet, regimen, the possibility of dialysis and other measures. Patients should be free from physical activity(protein catabolism increases), outdoor exposure is recommended. The basis of treatment is a proper diet.
Diet
Treatment of chronic renal failure begins with a properly selected diet:
- fractional food, 4-5 times a day;
- it is required to limit protein to 50-70 grams per day;
- meet energy needs at the expense of fats and carbohydrates;
- regulation of salt metabolism (restriction of salt).
In clinical nutrition for chronic renal failure exists. IN initial stage Diet No. 7 is enough, and for severe disorders, diets No. 7a or 7b are used (20 and 40 grams of protein per day).
In nutrition, it is advisable to arrange fasting days: rice - compote, carbohydrate apple - sugar, potato. Potatoes are cut raw and soaked to reduce potassium levels.
At the same time, 50% of daily dose protein should be easily digestible protein (cottage cheese or egg). But meat, fish, poultry, legumes, nuts and chocolate should be completely excluded. Marshmallow, marshmallow, honey and caramel are not forbidden. Dried fruits (except soaked) are contraindicated, as they contain an excess of potassium.
Fat is given in the form of vegetable oils. The amount of table salt is strictly taken into account and does not exceed 8 g per day. The amount of liquid in food and drink depends on the diuresis of the patient, and should not exceed it.
Drugs for the treatment of chronic renal failure
Drugs for the treatment of renal failure are symptomatic. We will not consider the treatment of diseases that led to CRF. To do this, patients may be prescribed serious medications, such as hormones and cytostatics. As for taking drugs to correct CRF itself, these include:
- antihypertensive drugs in the presence of malignant hypertension;
- diuretics and cardiac glycosides in violation of cardiac pumping function and the development of congestive heart failure;
- sodium bicarbonate for the relief of acidosis,
- iron preparations for anemia;
- antiemetics for nausea and vomiting ("Cerukal");
- enterosorbents to reduce azotemia ("Enteros-gel);
- bowel lavage, enemas.
In the treatment of chronic renal failure, at present, extracorporeal detoxification methods are “salvation”: hemosorption, plasmapheresis, as auxiliary methods, and chronic hemodialysis, or an “artificial kidney” apparatus. This allows you to save the life and activity of patients, and wait for a kidney transplant, if indicated.
But science does not stand still. In 2010, a prototype of an implantable artificial kidney was created, and the time is not far off when it will be possible to create a human kidney anew, using its stem cells, as well as the connective tissue base.
Forecast
We have only scratched the surface of the issues related to the causes, symptoms, and treatment of chronic kidney disease. The main thing to remember is that CRF is a non-specific syndrome that develops with many diseases.
Only the opportunity to reverse the course of the underlying disease gives a chance to stabilize the patient's condition. In addition, age, comorbidity, the possibility of dialysis, and the prospects for a kidney transplant must be taken into account.
kidney failure- a pathological condition that occurs when various diseases and is characterized by impaired renal function.
The kidney is an organ of the urinary system. Its main function is the formation of urine.  It happens like this:
It happens like this:
- Blood entering the kidney vessels from the aorta reaches the glomerulus of capillaries surrounded by a special capsule (Shumlyansky-Bowman capsule). Under high pressure, the liquid part of the blood (plasma) with the substances dissolved in it seeps into the capsule. This is how primary urine is formed.
- Then the primary urine moves through the system of convoluted tubules. Here, water and substances necessary for the body are absorbed back into the blood. Secondary urine is formed. Compared to the primary one, it loses in volume and becomes more concentrated, only harmful metabolic products remain in it: creatine, urea, uric acid.
- From the system of tubules, secondary urine enters the renal calyces, then into the pelvis and into the ureter.
- Excretion of harmful metabolic products from the body.
- Regulation of osmotic blood pressure.
- Hormone production. For example, renin, which is involved in the regulation of blood pressure.
- Regulation of the content of various ions in the blood.
- Participation in hematopoiesis. The kidneys excrete biologically active substance erythropoietin, which activates the formation of erythrocytes (red blood cells).
Causes of kidney failure
Causes of acute renal failure
Classification of acute renal failure, depending on the causes:- prerenal. Caused by impaired renal blood flow. The kidney does not receive enough blood. As a result, the process of urine formation is disrupted, pathological changes occur in the renal tissue. It occurs in about half (55%) of patients.
- Renal. Associated with pathology of the renal tissue. The kidney receives enough blood, but cannot form urine. Occurs in 40% of patients.
- Postrenal. Urine is formed in the kidneys, but cannot flow due to an obstruction in the urethra. If an obstruction occurs in one ureter, then the healthy kidney will take over the function of the affected kidney - renal failure will not occur. This condition occurs in 5% of patients.
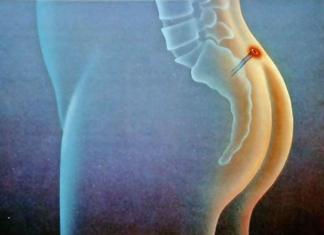
 In the picture: A - prerenal renal failure; B - postrenal renal failure; C - renal renal failure.
In the picture: A - prerenal renal failure; B - postrenal renal failure; C - renal renal failure.Causes of acute renal failure:
| prerenal |
|
| Renal |
|
| Postrenal |
|
Causes of chronic renal failure

Symptoms of kidney failure
Symptoms of acute renal failure
Symptoms of acute renal failure depend on the stage:- initial stage;
- the stage of reducing the daily volume of urine less than 400 ml (oliguric stage);
- the stage of restoring the volume of urine (polyuric stage);
- full recovery stage.
| Stage | Symptoms |
| Initial | At this stage, as such, there is no renal failure yet. A person is concerned about the symptoms of the underlying disease. But disturbances in the renal tissue are already occurring. |
| oliguric | Kidney dysfunction increases, the amount of urine decreases. Due to this, harmful metabolic products are retained in the body, there are violations of the water-salt balance. Symptoms:
|
| polyuric | The patient's condition returns to normal, the amount of urine increases, as a rule, even more than normal. At this stage, dehydration of the body, infections can develop. |
| Full recovery | Final restoration of kidney function. Usually lasts from 6 to 12 months. If during acute renal failure a large part of the kidney tissue was turned off from work, then complete recovery is impossible. |
Symptoms of chronic renal failure

- At the initial stage, chronic renal failure has no manifestations. The patient feels relatively normal. Usually, the first symptoms appear when 80% -90% of the kidney tissue ceases to function. But before that time, you can establish a diagnosis if you conduct an examination.
- Usually appear first general symptoms: lethargy, weakness, increased fatigue, frequent malaise.
- The excretion of urine is impaired. In a day, it is formed more than expected (2-4 liters). This can lead to dehydration. There is frequent urination at night. In the later stages of chronic renal failure, the amount of urine decreases sharply - this bad sign.
- Nausea and vomiting.
- Muscle twitches.
- Skin itching.
- Dryness and bitterness in the mouth.
- Stomach ache.
- Diarrhea.
- Nose, stomach bleeding due to decreased blood clotting.
- Hemorrhages on the skin.
- Increased susceptibility to infections. These patients often suffer respiratory infections, pneumonia .
- In the late stage: the condition worsens. There are attacks of shortness of breath, bronchial asthma. The patient may lose consciousness, fall into a coma.
Diagnosis of kidney failure
| Diagnostic method | Acute renal failure | Chronic renal failure |
| General urine analysis | In the general analysis of urine in acute and chronic renal failure, one can identify:
 |
|
| Bacteriological examination of urine | If the kidney dysfunction was caused by an infection, then the pathogen will be detected during the study. Also, this analysis allows you to identify an infection that has arisen against the background of renal failure, to determine the sensitivity of the pathogen to antibacterial drugs.  |
|
| General blood analysis | In acute and chronic renal failure in the general blood test, changes are detected:
 |
|
| Blood chemistry | Helps to assess pathological changes in the body due to impaired renal function. In a biochemical blood test in acute renal failure, changes can be detected:
| In chronic renal failure in a biochemical blood test, changes are usually detected:
|
| These methods allow you to examine the kidneys, their internal structure, renal calyces, pelvis, ureters, bladder. In acute renal failure, CT, MRI, and ultrasound are most commonly used to find the cause of urinary tract narrowing.  |
|
| Doppler ultrasound | Ultrasound examination, during which it is possible to evaluate the blood flow in the vessels of the kidneys. | |
| Radiography chest | It is used to detect disorders of the respiratory system, some diseases that may cause kidney failure.
|
|
| Chromocystoscopy |
| |
| Kidney biopsy | The doctor receives a piece of kidney tissue and sends it to a laboratory for examination under a microscope. Most often this is done with a special thick needle, which the doctor inserts into the kidney through the skin. Biopsy is used in doubtful cases when the diagnosis cannot be established.
|
|
| Electrocardiography (ECG) | This study is mandatory for all patients with acute renal failure. It helps to identify violations of the heart, arrhythmia.  |
|
| Zimnitsky's test | The patient collects all urine during the day in 8 containers (each for 3 hours). Determine its density and volume. The doctor can assess the state of kidney function, the ratio of daytime and nighttime urine volumes. | |
Treatment of kidney failure
 Acute renal failure requires immediate hospitalization of the patient in a nephrological hospital. If the patient is in serious condition, he is placed in the intensive care unit. Therapy depends on the causes of impaired renal function.
Acute renal failure requires immediate hospitalization of the patient in a nephrological hospital. If the patient is in serious condition, he is placed in the intensive care unit. Therapy depends on the causes of impaired renal function. In chronic renal failure, therapy depends on the stage. At the initial stage, the underlying disease is treated - this will help prevent severe renal dysfunction and make it easier to deal with them later. With a decrease in the amount of urine and the appearance of signs of kidney failure, it is necessary to deal with pathological changes in the body. And during the recovery period, you need to eliminate the consequences.
Directions for treatment of renal failure:
| Direction of treatment | Events |
| Elimination of the causes of prerenal acute renal failure. |
|
| Elimination of the causes of renal acute renal failure |
|
| Elimination of the causes of postrenal acute renal failure | It is necessary to eliminate the obstacle that interferes with the outflow of urine (tumors, stones, etc.). Most often, this requires surgical intervention. |
| Elimination of the causes of chronic renal failure | Depends on the underlying disease. |
| Measures to combat disorders that occur in the body in acute renal failure |
|
| Elimination of violations of the water-salt balance |
|
| The fight against acidification of the blood | The doctor prescribes treatment in the case when the acidity (pH) of the blood falls below the critical value - 7.2. A solution of sodium bicarbonate is administered intravenously until its concentration in the blood rises to certain values, and the pH rises to 7.35. |
| Fighting anemia | With a decrease in the level of red blood cells and hemoglobin in the blood, the doctor prescribes blood transfusions, epoetin (a drug that is an analogue of the renal hormone erythropoietin and activates hematopoiesis). |
| Hemodialysis, peritoneal dialysis | Hemodialysis and peritoneal dialysis are methods of cleansing the blood of various toxins and unwanted substances. Indications for acute renal failure:
In peritoneal dialysis, a blood purification solution is injected into abdominal cavity. As a result of the difference in osmotic pressure, it takes in harmful substances. It is then removed from the abdomen or replaced with a new one.
|
| kidney transplant | Kidney transplantation is carried out in chronic renal failure, when severe disorders occur in the patient's body, and it becomes clear that it will not be possible to help the patient in other ways. A kidney is taken from a living donor or a corpse. After transplantation, a course of therapy with drugs that suppress the immune system is carried out so that there is no rejection of the donor tissue.
|
Diet for acute renal failure

Prognosis for renal failure
Prognosis for acute renal failure
Depending on the severity of acute renal failure and the presence of complications, 25% to 50% of patients die.Most common causes death:
- Defeat nervous system- uremic coma.
- Severe circulatory disorders.
- Sepsis is a generalized infection, "blood poisoning", in which all organs and systems suffer.
Prognosis for chronic renal failure
Depends on the disease, against which there was a violation of kidney function, age, condition of the patient's body. Since the use of hemodialysis and kidney transplantation, the death of patients has become less common.Factors that worsen the course of chronic renal failure:
- arterial hypertension;
- improper diet, when food contains a lot of phosphorus and protein;
- high protein content in the blood;
- increased function of the parathyroid glands.
- kidney injury;
- urinary tract infection;
- dehydration.
Prevention of chronic renal failure
If you start early proper treatment a disease that can lead to chronic kidney failure, then kidney function may not be affected, or at least its impairment will not be so severe.Some medications are toxic to renal tissue and can lead to chronic renal failure. Do not take any medications without a doctor's prescription.
Most often, renal failure develops in people suffering from diabetes mellitus, glomerulonephritis, arterial hypertension. Such patients need to be constantly monitored by a doctor, timely undergo examinations.
Kidney disease is a dangerous condition that leads to a decrease in the quality of life and entails dangerous complications up to and including death. The most common is acute renal failure.
Acute renal failure (ARF) is a disease that occurs when one or two kidneys stop functioning or decrease in efficiency. The disease develops rapidly, accompanied by a sharp deterioration in the patient's condition and the development of severe intoxication. According to the international classification of diseases, the diagnosis of acute renal failure microbial 10 is assigned class N17.
When diagnosed with acute renal failure, symptoms begin to appear fairly quickly. There are several stages of the disease, each of which has a peculiar course and is characterized by a certain condition of the patient.
Initial - lasts from 2-3 hours to 3 days. The patient experiences weakness, drowsiness, dyspeptic disorders may appear in the form of nausea or indigestion. There are no specific signs.
Oligoanuric - characterized by a sharp decrease in the volume of urine, a change in its color. There is a protein in the OAM, the acetonomic syndrome develops. The blood contains a high content of nitrogen, phosphates, sodium and potassium. Severe intoxication develops, up to a coma, and general immunity decreases.
Popyuric - a decrease in the daily volume of urine is sharply replaced by its increase, hypotension develops due to the leaching of useful minerals, including potassium. Perhaps the development of arrhythmias. With a favorable course and appropriate treatment, within a week the symptoms subside, there is an improvement in the condition and blood counts.
The recovery phase - lasts up to a year, consists in the complete restoration of kidney function. Provided that preventive measures are followed, the outcomes are favorable.
Depending on the causes caused by the disease, the following types of acute renal failure are distinguished:
Prerenal acute renal failure - characterized by a sharp slowdown in renal blood flow. The reasons include:
- cardiovascular diseases;
- cardiac arrhythmia syndrome;
- blockage of the pulmonary artery;
- severe dehydration;
- cardiogenic shock.

Renal acute renal failure - characterized by a sharp release of toxic substances, due to ischemic damage to the tissues of the kidneys. Causes:
- poisoning with pesticides;
- excessive use of a number of drugs, including antibiotics;
- increased content of hemoglobin in the blood;
- acute pyelonephritis and other inflammatory diseases.
Postreal acute renal failure - caused by obstruction of the urinary tract, the causes of which are:
- neoplastic diseases internal organs;
- urethritis;
- narrowing of the paths due to the abundance of stones.
The causes of acute renal failure are varied. In addition to all of the above, a disease can occur due to the penetration of bacteria from other organs, therefore, even a common ARVI can lead to the development of the disease.
Diagnosis of the disease
Since the primary signs of renal failure can easily be confused with the symptoms of other diseases, special laboratory tests and diagnostic measures should be performed to make a diagnosis. At the examination, the doctor will collect a personal and family analysis, examine the condition skin, determine the presence of concomitant somatic diseases, listen to the heartbeat, assess the state of the lymphatic system.
Next, carry out general analysis urine and biochemical analysis blood. There is a drop in hemoglobin, the development of leukocytosis and lymphopenia. According to biochemistry, a decrease in hematocrit is diagnosed, which indicates hyperhydration. In addition, there is an increase in the level of urea up to 6.6 mmol/l and creatinine - up to 1.45 mmol/l. An increased content of calcium, potassium, sodium, phosphate, a decrease in acidity can be detected.

Hyaline and granular casts are found in the urine, erythrocytes and leukocytes increase, and the specific gravity decreases significantly. An increase in the level of eosinophils in acute nephritis is possible. When diagnosed with acute renal failure, the pathogenesis depends on the causative agent of the disease and the form of the disease. To determine it, as well as to confirm or refute acute renal failure, an ultrasound examination of the kidneys and bladder is performed. There is an increase in the volume of internal organs, the presence of stones in the pelvis and urinary tract.
For a better study, cystoscopy (examination of the bladder) and ureteroscopy (endoscopy of the urethra), as well as radionuclide research methods are performed to assess the condition of the internal organs by introducing a contrast agent.
In addition, a study of the heart, ECG, CT, MRI, angiography, chest x-ray (to exclude accumulation of fluid in the pleura of the lungs), radioisotope scanning of the kidneys is carried out. In especially severe cases, a biopsy and bilateral catherization of the pelvis may be recommended.
Features of treatment
When diagnosed with acute renal failure, treatment is prescribed immediately. The drugs prescribed for the disease are determined by the types and stages of the disease.
In the initial stage of acute renal failure, the treatment of a concomitant disease that caused dysfunction of the kidneys is taken as the basis. In the case of cardiogenic shock, therapy is prescribed aimed at normalizing cardiac activity, eliminating arrhythmias and restoring blood flow. With chemical or food poisoning relieve acute intoxication syndromes. If there are stones in the pelvis, they are cleaned, and methods are also used to get rid of stones. In the event that the clinic of the disease obliges, antitumor therapy is prescribed.

If the disease is diagnosed at the stage of oliguria, the patient is prescribed diuretics, in particular furasimide, mannitol, a 20% glucose solution and insulin. To prevent dehydration, dopamine is administered intravenously to the patient, as well as other drugs that restore the electrolyte balance of the blood. With severe inflammatory processes antibiotics are prescribed. All treatment is carried out exclusively in a hospital to prevent the development of complications and the occurrence side effects. The patient is also advised to healthy lifestyle life and follow a special diet with a reduced content of proteins and salts.
If the clinic of the disease is characterized by manifestations dangerous symptoms, surgery or connection to a hemodialysis system is recommended. The latter is used in case of persistent developed intoxication of the body, if the level of urea in the analyzes rises to 24 mmol / l, and potassium is diagnosed at the level of 7 mmol / l. In addition, the procedure of dialysis is indicated in case of inefficiency. conservative therapy, a serious condition of the patient, a state of chronic ketocidosis.
Features of the course of the disease in children
Acute renal failure in children is a rare disease, but very dangerous. Not so long ago it had a very Negative consequences up to death. The disease manifests itself as a sudden deterioration in well-being, electrolyte imbalance, severe intoxication and headache and is characterized by hypoxia of the renal tissues, as well as damage to the tubules.
Acute renal failure develops in children against the background of diseases such as:
- nephritis;
- infectious diseases urinary system;
- toxic shock;
- intrauterine infections and hypoxia;
- hemoglobin and myoglobinuria;
- renal ischemia.
Also, a predisposition to the onset of the disease can be banal hypothermia, suffocation, respiratory failure, asphyxia - in newborns. In young patients, two forms of the disease are distinguished: functional and organic.

Functional acute renal failure in children occurs against the background of dehydration and impaired blood flow through the vessels. This form of the disease is poorly diagnosed, however, is reversible. The most dangerous is the organic form of the disease. The disease, manifested by lethargy, pallor and dryness of the skin, has pronounced symptoms.
There is a low amount of urine, nausea, dizziness, vomiting and tachycardia may occur, a developing acetonomic syndrome often occurs, manifested by uncontrollable vomiting and severe dehydration. In especially severe cases, moist rales are heard in the lungs, there is a risk of developing uremic coma.
If at least one of the symptoms appears, the child must be immediately hospitalized. Urgent Care in acute renal failure will be provided immediately. It includes measures to restore electrolyte balance, fluid compensation in the body. Treatment is also prescribed for the underlying disease that caused the problem in the kidneys.
Rest medical measures children are no different from adults. It is important to cure the disease to the end, and not let everything take its course after the disappearance of the main symptoms. On average, treatment severe forms in young patients lasts 3-6 months. If the kidney function is not fully restored, a chronic form of the disease may develop.
Chronic renal failure
If the acute form of the disease could not be cured completely by removing all possible reasons, and kidney dysfunction is observed for 3 months or more, a chronic form of the disease develops. Its symptoms slowly increase, ranging from excessive weakness and fatigue of the patient to the development of cardiac asthma and pulmonary edema. Other symptoms of chronic kidney disease include:
- dryness and bitterness in the mouth;
- frequent convulsions;
- loss of appetite;
- pain in the lower back;
- frequent headaches and pressure drops.
During illness, internal bleeding may develop, the body's resistance to various infections may decrease, frequent dizziness is possible, up to loss of consciousness. Causes of chronic renal failure include diabetes, various infectious diseases, diseases of the cardiovascular system, chronic glomerulonephritis, urolithiasis disease, polycystic kidney disease, poisoning with toxic products.

Acute and chronic renal failure is diagnosed in the same way, with the caveat that in the chronic form of the disease, the indicators may not be so high, but last longer. The treatment is also similar. If the disease progresses rapidly, the doctor may recommend removal of the non-functioning kidney or hemodialysis and peritoneal dialysis procedures.
The difference between the latter is that during hemodialysis, the blood plasma is periodically filtered through the “artificial kidney” apparatus in order to purify the blood and remove toxins, and during peritoneal dialysis, the purification occurs directly through the patient’s peritoneum using a special catheter that conducts dialysis solution into the patient’s blood.
diet for kidney failure
Treatment of any form of renal failure is impossible without a special diet. Since the disease is associated with disruption of the kidneys, the diet for acute renal failure is characterized by a decrease in protein (up to 50 grams per day), salt, and the consumption of fatty, spicy, fried foods should also be limited.
The food is high in calories, rich in healthy fats and carbohydrates. Do not neglect fresh vegetables and fruits, use berry fruit drinks, juices and compotes, it is also recommended to include whole grain bread in the diet, as well as pastries based on corn and rice flour.

The diet is based on cereals, soups, vegetable stews, low-fat broths, legumes, nuts, dried fruits are acceptable. In limited quantities, it is possible to consume fatty fish, caviar, dairy products, seeds, eggs.
- drinks containing caffeine;
- chocolate;
- rich bone and meat broths;
- alcoholic drinks;
- hot spices;
- smoked and canned foods;
- mushrooms.
Otherwise, nutrition in acute and chronic renal failure should be selected individually for each patient. It should be noted that during periods of exacerbation, one should tighten the diet, completely remove salt, reduce the amount of proteins to 20 grams per day, and the use of animal proteins is more likely than vegetable proteins. That is why in the acute form of the disease one should not lean on beans, various nuts and dried fruits. However, food is supposed to be fun, so it's worth experimenting with recipes to get delicious meals from the available ingredients.
Complications of kidney failure
Complications in acute and chronic renal failure develop in the absence of timely treatment and failure to follow the recommendations of a specialist.
When acute form, the level of risk depends on the degree of the disease, the state of catabolism, the presence of oliguria and nephrotic syndrome. In this case, there is a risk of serious poisoning by metabolic products and minerals, the concentration in the blood of which is steadily increasing. Without proper attention, hyperkalemia develops in acute renal failure. Having reached critical values, this condition can lead to serious heart problems, up to and including death.

Diseases can cause severe changes in the blood, causing anemia or causing immune disorders. Patients with a chronic form of the disease must be extremely careful and avoid contact with unhealthy people. Their body, more than others, is susceptible to infection, which can rapidly develop and lead to the death of the patient.
It is also possible the development of neurological diseases and the occurrence of acute heart failure. In severe cases of acute renal failure, gastroenterocolitis develops, causing intestinal bleeding, which further complicates the patient's condition.
When chronic form diseases, there is an active leaching of calcium from the body, which leads to increased bone fragility. On the part of neurology, frequent seizures, complete or partial loss of consciousness, and mental retardation may occur. Pregnant women with chronic renal failure require special attention. The development of the disease or the occurrence of an exacerbation can lead to termination of pregnancy and a threat to the life of the mother.
Disease prevention
If the symptoms of the acute form of the disease are stopped or the period of exacerbation in chronic patients is removed, the patient should take a whole range of measures so that the disease does not return soon or even recedes:
- Follow a strict diet. Even if there is a stable improvement, you should not lean on protein foods. And, if the patient still allows himself meat, then let it be boiled or baked, well, by no means smoked or spicy.
- Give up alcohol or reduce its consumption.
- Limit your intake of caffeinated drinks.
- Maintain weight. If the condition allows, you should go in for sports or at least walk more in the fresh air.
- Carefully follow all the recommendations of the attending physician, without gaps, take all the drugs prescribed for treatment.
- Give up smoking.
- Avoid being in smoky rooms, working with pesticides.
- Reduce the risk of any exposure to toxins from outside.
- In the event of foci of inflammation in any area of the body, immediately stop them, in order to avoid the spread of infection.
Acute renal failure is dangerous disease leading to serious malfunctions of the body, up to death. No one is immune from illness. But it is possible to get rid of complications. The main thing is to contact a narrow specialist in time and follow all the recommendations not only in the stage of exacerbation, but throughout the entire period of rehabilitation.
Acute renal failure (ARF) develops as a complication of many diseases and pathological processes. Acute renal failure is a syndrome that develops as a result of impaired renal processes (renal blood flow, glomerular filtration, tubular secretion, tubular reabsorption, renal concentrating ability) and is characterized by azotemia, disturbances in water and electrolyte balance and acid-base state.
Acute renal failure may be due to prerenal, renal, and postrenal disorders. Prerenal acute renal failure develops in connection with a violation of the renal blood flow, renal acute renal failure - with damage to the renal parenchyma, postrenal acute renal failure is associated with a violation of the outflow of urine.
The morphological substrate of ARF is acute tubulonecrosis, manifested by a decrease in the height of the brush border, a decrease in the folding of the basolateral membranes, and necrosis of the epithelium.
Prerenal acute renal failure is characterized by a decrease in renal blood flow as a result of vasoconstriction of afferent arterioles in conditions of impaired systemic hemodynamics and a decrease in circulating blood volume, while kidney function is preserved.
Causes of prerenal renal failure:
long-term or short-term (less often) decrease in blood pressure below 80 mm Hg. (shock due to various reasons: post-hemorrhagic, traumatic, cardiogenic, septic, anaphylactic, etc., extensive surgical interventions);
decrease in the volume of circulating blood (blood loss, plasma loss, indomitable vomiting, diarrhea);
an increase in intravascular capacity, accompanied by a decrease in peripheral resistance (septicemia, endotoxemia, anaphylaxis);
decrease in cardiac output ( myocardial infarction, heart failure, pulmonary embolism).
The key link in the pathogenesis of prerenal acute renal failure is a sharp decline the level of glomerular filtration due to spasm of afferent arterioles, shunting of blood in the juxtaglomerular layer and ischemia of the cortical layer under the influence of a damaging factor. Due to a decrease in the volume of blood perfused through the kidneys, the clearance of metabolites decreases and develops azotemia. Therefore, some authors call this type of OPN prerenal azotemia. With a prolonged decrease in renal blood flow (more than 3 days) prerenal acute renal failure turns into renal acute renal failure.
The degree of renal ischemia correlates with structural changes in the epithelium of the proximal tubules (decrease in the height of the brush border and the area of the basolateral membranes). Initial ischemia promotes an increase in the permeability of tubular epithelium cell membranes for [Ca2+] ions, which enter the cytoplasm and are actively transported by a special carrier to the inner surface of mitochondrial membranes or to the sarcoplasmic reticulum. The energy deficit developing in cells due to ischemia and energy consumption during the movement of [Ca 2+ ] ions leads to cell necrosis, and the resulting cellular debris obstructs the tubules, thereby aggravating anuria. The volume of tubular fluid in conditions of ischemia is reduced.
Damage to nephrocytes is accompanied by a violation of sodium reabsorption in the proximal tubules and an excessive intake of sodium in the distal regions. Sodium stimulates macula densa renin production; in patients with acute renal failure, its content is usually increased. Renin activates the renin-angiotensin-aldosterone system. The tone of the sympathetic nerves and the production of catecholamines are increased. Under the influence of the components of the renin-apgiotensin-aldosterone system and catecholamines, afferent vasoconstriction and renal ischemia are maintained. In the capillaries of the glomeruli, the pressure drops and, accordingly, the effective filtration pressure decreases.
With a sharp restriction of perfusion of the cortical layer, blood enters the capillaries of the juxtaglomerular zone ("Oxford shunt"), in which stasis occurs. An increase in pressure in the tubules is accompanied by a decrease in glomerular filtration. Hypoxia of the distal tubules most sensitive to it is manifested by necrosis of the tubular epithelium and basement membrane up to tubular necrosis. There is an obturation of the tubules by fragments of necrotic epithelial cells, cylinders, etc.
Under conditions of hypoxia in the medulla, a change in the activity of enzymes of the arachidonic cascade is accompanied by a decrease in the formation of prostaglandins that have a vasodilatory effect, and the release of biologically active substances (histamine, serotonin, bradykinin), which directly affect the kidney vessels and disrupt renal hemodynamics. This, in turn, contributes to secondary damage to the renal tubules.
After the restoration of renal blood flow, the formation of active forms of oxygen, free radicals and activation of phospholipase occurs, which maintains impaired membrane permeability for [Ca 2+ ] ions and prolongs the oliguric phase of acute renal failure. In recent years, calcium channel blockers (nifedipine, verapamil) have been used to eliminate unwanted calcium transport into cells in the early stages of acute renal failure, even against the background of ischemia or immediately after its elimination. A synergistic effect is observed when calcium channel inhibitors are used in combination with substances that can trap free radicals, such as glutathione. Ions, adenine nucleotides protect mitochondria from damage.
The degree of renal ischemia correlates with structural changes in the epithelium of the tubules, the development of vacuolar degeneration or necrosis of individual nephrocytes is possible. Vacuolar degeneration is eliminated within 15 days after the termination of the damaging factor.
Renal acute renal failure develops due to ischemia of the kidney, that is, it occurs a second time with a primary impaired perfusion of the kidney or under the influence of the following reasons:
inflammatory process in the kidneys (glomerulonephritis, interstitial nephritis, vasculitis);
endo- and exotoxins (drugs, radiopaque substances, salts of heavy metals - compounds of mercury, lead, arsenic, cadmium, etc., organic solvents, ethylene glycol, carbon tetrachloride, poisons of animal and vegetable origin;
renovascular diseases (thrombosis and embolism of the renal artery, dissecting aortic aneurysm, bilateral thrombosis of the renal veins);
pigmentemia - hemoglobinemia (intravascular hemolysis) and myoglobinemia (traumatic and non-traumatic rhabdomyolysis);
toxicosis of pregnancy;
hepatorenal syndrome.
This type of AKI is characterized by acute tubular necrosis caused by ischemia or nephrotoxins that are fixed on the cells of the renal tubules. First of all, the proximal tubules are damaged, dystrophy and necrosis of the epithelium occurs, followed by moderate changes in the interstitium of the kidneys. Glomerular lesions are usually minor.
To date, more than 100 nephrotoxins have been described that have a direct damaging effect on the cells of the renal tubules (acute tubular necrosis, nephrosis of the lower nephron, vasomotor vasopathy). Acute renal failure caused by nephrotoxins accounts for about 10% of all admissions of patients to acute hemodialysis centers.
Nephrotoxins cause damage to tubuloepithelial structures of varying severity - from dystrophies (hydropic, vacuole, balloon, fatty, hyalinodroplet) to partial or massive coagulative necrosis of nephrocytes. These changes occur as a result of reabsorption and deposition of macro- and microparticles in the cytoplasm, as well as fixation on the cell membrane and in the cytoplasm of nephrotoxins filtered through the glomerular filter. The occurrence of a particular dystrophy is determined by the acting factor.
nephrotoxicity of poisons thiol group"(compounds of mercury, chromium, copper, gold, cobalt, zinc, lead, bismuth, lithium, uranium, cadmium and arsenic) is manifested by the blockade of sulfhydryl (thiol) groups of enzymatic and structural proteins and a plasma coagulating effect, which causes massive coagulation necrosis of the tubules. Sublimate causes selective damage to the kidneys - " sublimate nephrosis". Other substances in this group do not differ in selectivity of action and damage the tissue of the kidneys, liver and red blood cells. For example, a feature of poisoning with copper sulphate, dichromates, arsenic hydrogen is a combination of coagulation necrosis of the epithelium of the proximal tubules with acute hemoglobinuric nephrosis. In case of poisoning with dichromates and arsenic hydrogen, centrilobular necrosis of the liver with cholemia and chelaturia is observed.
Poisoning ethylene glycol and its derivatives is characterized by irreversible destruction of intracellular structures, called balloon dystrophy. Ethylene glycol and its decay products are reabsorbed by the epithelial cells of the renal tubules, a large vacuole is formed in them, which displaces the cell organelles, together with the nucleus, to the basal regions. Such dystrophy, as a rule, ends with colliquat necrosis and complete loss of the function of the affected tubules. Sequestration of the damaged part of the cell together with the vacuole is also possible, and the preserved basal sections with the pushed out nucleus can be a source of regeneration.
Poisoning dichloroethane, less often chloroform, accompanied fatty degeneration nephrocytes (acute lipid nephrosis) of the proximal, distal tubules and the loop of Henle. These poisons have a direct toxic effect on the cytoplasm, changing the ratio of protein-lipid complexes in it, which is accompanied by inhibition of reabsorption in the tubules.
Reabsorption of protein pigment aggregates (hemoglobin, myoglobin) epithelial cells of the proximal and distal tubules causes hyalino-droplet dystrophy. Pigment proteins filtered through the glomerular filter move along the tubule and gradually deposited on the brush border in the proximal tubules, partially reabsorbed by nephrocytes. The accumulation of pigment granules in epithelial cells is accompanied by partial destruction of the apical sections of the cytoplasm and their sequestration into the lumen of the tubules along with the brush border, where granular and lumpy pigment cylinders are formed. The process unfolds over 3-7 days. During this period, non-reabsorbed pigment masses in the lumen of the tubules become denser, move into the loop of Henle and the distal tubules. In the apical sections of epithelial cells overloaded with pigment granules, partial necrosis occurs. Individual pigment granules are converted into ferritin and are retained for a long time in the cytoplasm.
Nephrotoxicity aminoglycosides(kanamycin, gentamicin, monomycin, neomycin, tobarmycin, etc.) is associated with the presence of free amino groups in the side chains in their molecules. Aminoglycosides are not metabolized in the body, and 99% of them are excreted unchanged in the urine. Filtered aminoglycosides are fixed on the apical membrane of the cells of the proximal tubules and the loop of Henle, bind to vesicles, are absorbed by pinocytosis, and are sequestered in the lysosomes of the tubular epithelium. At the same time, the concentration of the drug in the cortical substance becomes higher than in plasma. Damage to the kidneys by aminoglycosides is characterized by an increase in anionic phospholipids in the membranes, in particular, phosphatidylinositol, damage to mitochondrial membranes, accompanied by a loss of intracellular potassium and magnesium, impaired oxidative phosphorylation and energy deficiency. The combination of these changes leads to necrosis of the tubular epithelium.
Characteristically, [Ca 2+ ] ions prevent the fixation of aminoglycosides on the brush border and thus reduce their nephrotoxicity. It was noted that the tubular epithelium, regenerating after damage by aminoglycosides, becomes resistant to the toxic effects of these drugs.
Therapy osmotic diuretins(solutions of glucose, urea, dextrans, mannitol, etc.) can be complicated by hydropic and vacuolar degeneration of nephrocytes. At the same time, the osmotic gradient of fluids on both sides of the tubular cell changes in the proximal tubules - blood washing the tubules and provisional urine. Therefore, it is possible for water to move into tubular epithelial cells from peritubular capillaries or from provisional urine. Hydropia of epithelial cells with the use of osmotic diuretins persists for a long time and, as a rule, is associated with partial reabsorption of osmotically active substances and their retention in the cytoplasm. Water retention in the cell dramatically reduces its energy potential and functionality. Thus, osmotic nephrosis is not the cause of acute renal failure, but an undesirable effect of its treatment or a consequence of the replenishment of energy substrates in the body by parenteral administration of hypertonic solutions.
The composition of urine in renal acute renal failure is similar in composition to the glomerular filtrate: low specific gravity, low osmolarity. The content in the urine is increased due to a violation of its reabsorption.
Postrenal acute renal failure occurs due to a violation of the outflow of urine through the urinary tract as a result of the following disorders:
occlusion of the urinary tract with stones or blood clots;
obstruction of the ureters or ureter by a tumor located outside the urinary tract;
kidney tumors;
papilla necrosis;
prostate hypertrophy.
Violation of the outflow of urine is accompanied by overstretching of the urinary tract (ureters, pelvis, calyces, collecting ducts, tubules) and the inclusion of the reflux system. Backflow of urine from the urinary tract into the interstitial space of the renal parenchyma occurs (pyelorenal reflux). But pronounced edema is not observed due to the outflow of fluid through the system of venous and lymphatic vessels. (pyelovenous reflux). Therefore, the intensity of hydrostatic pressure on the tubules and glomerulus is very moderate, and filtration is reduced slightly. There are no pronounced disorders of the peritubular blood flow, and, despite anuria, renal function is preserved. After removing the obstruction to the outflow of urine, diuresis is restored. If the duration of occlusion does not exceed three days, the phenomena of acute renal failure after the restoration of the patency of the urinary tract disappear quickly enough.
With prolonged occlusion and high hydrostatic pressure, filtration and peritubular blood flow are disturbed. These changes, combined with persistent refluxes, contribute to the development of interstitial edema and tubular necrosis.
Clinical course of acute renal failure has a certain regularity and staging, regardless of the cause that caused it.
1st stage- short in duration and ends after the termination of the factor;
2nd stage - the period of oligoanuria (the volume of urine excreted does not exceed 500 ml / day), azotemia; in case of prolonged oliguria (up to 4 weeks) sharply increases the likelihood of cortical necrosis;
3rd stage- period of polyuria - restoration of diuresis with a phase of polyuria (the volume of urine excreted exceeds 1800 ml / day);
4th stage- restoration of kidney function. Clinically, the 2nd stage is the most difficult.
Extracellular and intracellular hyperhydration develops, non-gas excretory renal acidosis (depending on the localization of tubular damage, acidosis of the 1st, 2nd, 3rd types is possible). The first sign of overhydration is shortness of breath due to interstitial or cardiogenic pulmonary edema. A little later, the fluid begins to accumulate in the cavities, hydrothorax, ascites, edema of the lower extremities and in the lumbar region occur. This is accompanied by pronounced changes in blood biochemical parameters: azotemia (the content of creatinine, urea, uric acid is increased), hyperkalemia, hyponatremia, hypochloremia, hypermagnesemia, hyperphosphatemia.
The level of blood creatinine rises regardless of the nature of the patient's diet and the intensity of protein breakdown. Therefore, the degree of creatinemia gives an idea of the severity of the course and prognosis in acute renal failure. The degree of catabolism and necrosis of muscle tissue reflects hyperuricemia.
Hyperkalemia occurs as a result of a decrease in potassium excretion, an increased release of potassium from cells, and developing renal acidosis. Hyperkalemia 7.6 mmol / l is clinically manifested by cardiac arrhythmias up to complete cardiac arrest; hyporeflexia occurs, muscle excitability decreases with subsequent development of muscle paralysis.
Electrocardiographic indicators in hyperkalemia: T wave - high, narrow, ST line merges with T wave; disappearance of the P wave; widening of the QRS complex.
Hyperphosphatemia is caused by impaired phosphate excretion. The origin of hypocalcemia remains unclear. As a rule, shifts in phosphorus-calcium homeostasis are asymptomatic. But with the rapid correction of acidosis in patients with hypocalcemia, tetany and seizures may occur. Hyponatremia is associated with water retention or excess water intake. There is no absolute sodium deficiency in the body. Hypersulfatemia, hypermagnesemia, as a rule, are asymptomatic.
Within a few days, anemia develops, the genesis of which is explained by hyperhydration, hemolysis of erythrocytes, bleeding, inhibition of erythropoietin production by toxins circulating in the blood. Usually anemia is combined with thrombocytopenia.
The second stage is characterized by the appearance of signs of uremia, while symptoms from the gastrointestinal tract (lack of appetite, nausea, vomiting, flatulence, diarrhea) predominate.
With the appointment of antibiotics at the beginning, the symptoms of diarrhea increase. Subsequently, diarrhea is replaced by constipation due to severe intestinal hypokinesia. In 10% of cases, gastrointestinal bleeding (erosion, ulcers of the gastrointestinal tract, bleeding disorders) is observed.
Timely prescribed therapy prevents the development of coma, uremic pericarditis.
During the oliguric stage (9-11 days), the urine is dark in color, proteinuria and cylindruria are expressed, natriuria does not exceed 50 mmol / l, urine osmolarity corresponds to plasma osmolarity. In 10% of patients with acute drug-induced interstitial nephritis, diuresis is preserved.
3rd stage characterized by the restoration of diuresis by the 12-15th day from the onset of the disease and polyuria (more than 2 l / day), which persists for 3-4 weeks. The genesis of polyuria is explained by the restoration of the filtration function of the kidneys and the insufficient concentration function of the tubules. In the polyuric stage, the body is unloaded from the fluid accumulated during the period of oliguria. Secondary dehydration, hypokalemia and hyponatremia are possible. The severity of proteinuria is reduced.
Table 6
Differential diagnosis of prerenal and renal acute renal failure
For the differential diagnosis of prerenal and renal acute renal failure, the index of the excreted fraction of sodium and the index of renal failure are calculated (including the data of Table 6).
Excreted sodium fraction (Na + ex)
Na + urine: Na + blood
Na + ex = ------,
Urine Cr: Blood Cr
where Na + urine and Na + blood - respectively, the content of Na + in urine and blood, and Cr urine and Cr blood - the content of creatinine in urine and blood
For prerenal acute renal failure, the index of excreted sodium fraction is less than 1, with acute tubular necrosis, the index is greater than 1.
Renal Insufficiency Index (RII):
IPN = ------ .
Urine Cr: Blood Cr
The disadvantage of these indicators is that in acute glomerulonephritis they are the same as in prerenal acute renal failure.
Pathogenetic ways of correction in acute renal failure: replenishment of BCC - plasma, protein solution, polyglycans, reopoliglyukin (under the control of CVP);
diuretics - mannitol, furosemide - wash out tubular detritus;
prevention of hyperkalemia - 16 units of insulin, 40% in 50 ml of glucose solution;
prevention of hypercalcemia - 10% in 20.0-30.0 ml of calcium gluconate solution (an increase in the level of ionized Ca 2+ reduces cell excitability);
elimination of acidosis - the introduction of sodium bicarbonate.
Thus, the treatment is aimed at eliminating shock, replenishing the volume of circulating blood, treating the syndrome of disseminated intravascular coagulation, preventing overhydration, correcting the acid-base and water-electrolyte balance, eliminating uremia.