The mitral valve blocks regurgitation of blood, that is, prevents its reverse flow. To do this, you need to close the hole between the left ventricle and the atrium, which happens when the valve leaflets close. Failure mitral valve manifests itself when the valves cannot completely close, then a gap remains in the hole, and reverse movement of blood becomes possible.
Almost half of people with heart disease have a similar disorder. In this case, mitral regurgitation is usually accompanied by other problems, these can be various stenoses, pathologies of large vessels.
Why does pathology develop?
Mitral valve insufficiency results from damage to the valve itself or to the heart structures. There can be quite a lot of reasons for this. Moreover, it can be acute or chronic and is caused by various problems and diseases.
As a result of damage to various structures of the heart, the valve copes with its function worse. Both the valve leaflets themselves and the muscles that ensure their operation, or the tendons that control the valve leaflets, can be damaged.
Causes of acute failure
- Changes and destruction in the tissues of the mitral ring
- Sash perforation,
- Chord breaks,
- Weakening and destruction of papillary muscles.
As a rule, the cause of all these damages is disease. The main and most common cause today is infective endocarditis. The inflammatory process in this disease can negatively affect the condition of the tissues of the mitral ring, valve leaflets, or lead to the destruction of the chordae tendineae.
Some systemic diseases, in particular lupus erythematosus, can lead to the same damage to cardiac structures. Degenerative processes, spreading to cardiovascular system, negatively affect the condition of all heart tissues.

As a result of all these diseases, damage occurs that prevents the valve from closing the leaflets normally due to their perforation, rupture, or because the damaged muscles and chords can no longer effectively control the operation of the mitral valve.
The same damage can occur due to trauma that may occur during heart surgery.
Other reasons acute failure.
- Tumor processes in the atrium;
- Rheumatic processes;
- Left ventricular failure.
Causes of chronic failure
- Tissue changes due to inflammatory processes;
- Degenerative processes;
- Infections;
- Structural changes;
- Hereditary factors.
The inflammatory process does not always cause acute changes; it is possible that it proceeds sluggishly, and tissue damage increases slowly, often unnoticed by the patient. The chronic form of the disease can be caused by the same diseases as the acute form. This is infective endocarditis, lupus erythematosus.
Among the degenerative processes that lead to this pathology, myxomatous degeneration, connective tissue diseases, and calcium deposits in the mitral valve area are most often noted.

Some heart diseases lead to structural changes that prevent normal operation valve apparatus. For example, as a result of a heart attack or endocarditis, the chordae or papillary muscles are damaged, which becomes the direct cause of the development of chronic failure. It can lead to the same consequences.
Hereditary pathologies are formed during intrauterine development due to negative influences on the mother’s body. They can also be caused by genetic disorders. Most often it is formed due to defects of the valve leaflets and pathology of large vessels.
Peculiarities
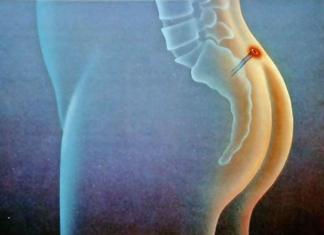
Hemodynamics with mitral insufficiency, that is, blood flow, depends on the severity of the pathology.
Degree of deficiency
- Minor;
- Moderate;
- Expressed;
- Heavy.
With a slight degree of regurgitation, it is observed directly at the mitral valve leaflets. It also occurs in healthy people. Moderate means regurgitation occurs one to one and a half centimeters from the valve.
In the third degree, the reverse movement of blood reaches the middle of the atrium. This leads to some expansion of the atrium. Severe insufficiency results in regurgitation occupying the entire left atrium.
How the problem manifests itself

The characteristic noise that the doctor notes when listening to the heart is the main symptom. It is caused by the return of blood from the left ventricle to the left atrium.
The diagnosis begins with this symptom. Although with mild deficiency there may be no symptoms.
With a more serious development of the defect, the left ventricle is forced to pump more blood in order to receive more blood that returns back to the atrium. As a result, it gradually increases and hypertrophies. At the same time, its contractions intensify, which is felt by a person as an increased heartbeat. These symptoms are especially noticeable when the patient lies on his left side.
Since blood returns to the atrium as a result of regurgitation, it must accommodate a larger volume of blood, and it also gradually increases. With a significant degree of enlargement, the atrium cannot cope with its function, because fibrillation and frequent irregular contractions occur. As a result, the pumping function of the heart decreases.
Further development of the degree of pathology leads to the fact that the atria do not contract normally at all, but only tremble. These problems can be fraught with more serious disorders, for example, the formation of blood clots, because there is no normal blood flow. Blood clots that form in the heart are very dangerous, because they can block large vessels, and this leads to damage various organs, stroke.
At grades 3 and 4, regurgitation can be quite pronounced, which puts additional stress on the heart. A person runs the risk of heart failure, which has symptoms such as shortness of breath, swelling, and cough. Damaged heart tissue becomes more vulnerable and less resistant to infection, so the risk of infective endocarditis increases.
A person with a moderate and severe degree does not have adequate blood supply to the organs, since such a disorder leads to a decrease in the pumping function of the heart. Since the organs do not receive normal nutrition, the entire body suffers, and this can affect its general condition and the well-being of the patient.
Symptoms
- Increased heart rate
- Increased fatigue
- Edema,
- Dyspnea,
- Cough,
- Cyanosis,
- Mitral flush.
Symptoms can appear in various combinations. If the problem is mild, there may be no obvious manifestations. A person may feel that he has become tired faster, has less time to do in a day, and is less able to tolerate physical activity.

All this is usually not perceived as symptoms of a heart problem, so the pathological process continues to progress.
Diagnostics
Diagnostic methods:
- Inspection;
- Urinalysis and blood analysis (general, biochemical, immunological);
- Doppler echocardiography;
- Ultrasound of the heart.
Other methods may be used to make a diagnosis, but these are the main ones and most often they are sufficient.
Examination and conversation with the patient make it possible to identify symptoms and suggest the presence of pathology. We need to find out what the person was sick with and what his heredity is. Analyzes allow us to determine the presence inflammatory process, cholesterol, sugar, blood protein levels and other important indicators. If antibodies are detected, it can suggest the presence of inflammation or infection in the heart muscle.
To make a diagnosis: an ECG is required, which shows the rhythm of the heart, helps to detect the presence of arrhythmia and other failures, assess whether there is an overload of the heart and whether its parts are enlarged. The main method is ultrasound or echocardiography.
Why do ultrasound of the heart?
- Assess the condition of the valve flaps;
- See how the doors close;
- Understand the sizes of the ventricles and atria;
- Measure the thickness of the heart walls;
- Detect thickening of the inner lining of the heart.
Doppler echocardiography is a test that shows how blood moves. This diagnostic method makes it possible to identify the reverse flow of blood, which is characteristic of such a defect.
How to treat the disease
If symptoms are identified and a diagnosis is made, then you need to find out the cause of the heart valve defect. First of all, you need to treat the disease that led to this condition. If the problem is mild or moderate, then, as a rule, additional treatment not required.

If the degree of damage is more serious or complications arise (heart failure, arrhythmia), then you will need drug treatment.
In case of severe deficiency, treatment must be comprehensive, and surgery may be required.
Surgically treated using operations performed with artificial circulation.
During plastic surgeries, which are performed at 2-3 degrees of the disease, a special support ring can be installed near the valves, the chords and valves are shortened. After the operation, blood flow is normalized, and the patient’s own valve is preserved.
If plastic surgery does not bring results or the tissues are severely damaged, then prosthetics are necessary. Biological or mechanical prostheses are used. For the manufacture of biological ones, animal tissues are used, mechanical ones are made from special alloys.
Features of the postoperative period
- Anticoagulant therapy is not required after plastic surgery.
- After implantation of a biological prosthesis, anticoagulants are required for 2-3 months.
- After installation of an artificial prosthesis, anticoagulants are prescribed for continuous use.
The success of treatment and how a person will feel after surgery depends on the degree of manifestations of insufficiency and regurgitation, on the dynamics of the disease and individual characteristics. It is important not to delay diagnosis and treatment.
The mitral valve is a valve located between the left atrium and the left ventricle of the heart that prevents regurgitation of blood into the left atrium during systole.
Mitral valve insufficiency or mitral regurgitation is the inability of the valve to prevent regurgitation of blood from the left ventricle into the left atrium.
Regurgitation is the rapid flow of blood in the direction opposite to normal movement, occurring during systole.
Mitral regurgitation rarely occurs in isolation (about 2% of the total number of heart diseases). It is accompanied by aortic valve defects and mitral stenosis.
There are functional (relative) and organic mitral insufficiency.
Functional mitral regurgitation is caused by acceleration of blood flow during dystonia, changes in the tone of papillary muscle fibers, dilatation (expansion) of the left ventricle, which provides hemodynamic overload of the heart.
Organic mitral regurgitation develops as a result of anatomical damage to the connective tissue plates of the valve itself, as well as the tendon strands that fix the valve.
Hemodynamic disorders of these types of mitral insufficiency are of the same nature.
Hemodynamic disturbances in various forms of mitral insufficiency
Systole is a series of successive contractions of the ventricular and atrium myocardium of a certain phase of the cardiac cycle.
Aortic pressure significantly exceeds left atrial pressure, which promotes regurgitation. During systole, reverse blood flow occurs in the left atrium, caused by incomplete covering of the atrioventricular orifice by the valve leaflets. As a result, an additional portion of blood enters diastole. During ventricular diastole, a significant volume of blood flows from the atrium into the left ventricle. As a result of this disorder, overload occurs on the left side of the heart, which increases the force of contraction of the heart muscle. Myocardial hyperfunction is observed. On initial stages development of mitral regurgitation, good compensation occurs.
Mitral regurgitation leads to hypertrophy of the left ventricle and left atrium, resulting in increased pressure in the pulmonary vessels. Spasm of the pulmonary arterioles causes pulmonary hypertension, resulting in the development of right ventricular hypertrophy and tricuspid valve insufficiency.
Mitral valve insufficiency: symptoms, diagnosis
With good compensation of mitral valve insufficiency, symptoms do not appear. Severe mitral regurgitation is characterized by the following symptoms:
- Shortness of breath and irregular heart rhythms during physical activity (then at rest);
- Cardialgia;
- Increased fatigue;
- Cardiac asthma (attacks of severe shortness of breath);
- Pain, swelling in the right hypochondrium, caused by an enlarged liver;
- Edema lower limbs;
- Dry cough with a small amount of sputum, in rare cases with blood;
- Pain in the heart area of a stabbing, pressing, aching nature, not associated with physical activity.
With compensated mitral valve insufficiency, symptoms may not appear for several years. The severity of symptoms is determined by the strength of regurgitation.
To diagnose mitral insufficiency, the following methods are used:
- An ECG can reveal signs of overload and hypertrophy of the left ventricle and atrium, and in the third stage - of the right heart;
- EchoCG - determination of hypertrophy and dilatation of the left heart;
- X-ray examination of organs chest– determination of the degree of pulmonary venous hypertension, the degree of protrusion of the atrial arches;
- Ventriculography – determining the presence and degree of regurgitation;
- Ventricular catheterization – determination of pressure dynamics in the ventricles of the heart.
Currently, there is an overdiagnosis of mitral insufficiency. Modern methods Studies have shown that a minimal degree of regurgitation may be present in a healthy body.
Mitral valve insufficiency 1st degree: clinical picture
Mitral valve insufficiency of the 1st degree is characterized by compensation of hemodynamics and the inability of the valve to prevent the reverse flow of blood, which is achieved by hyperfunction of the left ventricle and atrium. This stage of the disease is characterized by the absence of symptoms of circulatory failure and the patient’s well-being during physical activity. When diagnosing mitral valve insufficiency of the 1st degree, a slight expansion of the borders of the heart to the left, the presence systolic murmurs. There are no signs of valve dysfunction on the electrocardiogram.
Mitral valve insufficiency 2nd degree: clinical picture
 Mitral valve insufficiency of the 2nd degree is characterized by the development of a passive form of venous pulmonary hypertension. This stage is characterized by a number of symptoms of circulatory disorders: shortness of breath and rapid heartbeat during physical activity and at rest, cough, attacks of cardiac asthma, hemoptysis. When diagnosing mitral valve insufficiency of the 2nd degree, expansion of the borders of the heart to the left (1 - 2 cm), to the right (up to 0.5 cm) and upward, and systolic murmurs are detected. The electrocardiogram shows changes in the atrial component.
Mitral valve insufficiency of the 2nd degree is characterized by the development of a passive form of venous pulmonary hypertension. This stage is characterized by a number of symptoms of circulatory disorders: shortness of breath and rapid heartbeat during physical activity and at rest, cough, attacks of cardiac asthma, hemoptysis. When diagnosing mitral valve insufficiency of the 2nd degree, expansion of the borders of the heart to the left (1 - 2 cm), to the right (up to 0.5 cm) and upward, and systolic murmurs are detected. The electrocardiogram shows changes in the atrial component.
Mitral valve insufficiency 3rd degree: clinical picture
With mitral valve insufficiency of the 3rd degree, right ventricular hypertrophy develops, which is accompanied by characteristic symptoms: liver enlargement, development of edema, increased venous pressure.
Diagnosis of mitral valve insufficiency of the 3rd degree reveals a significant expansion of the boundaries of the heart muscle and intense systolic murmurs. An electrocardiogram shows the presence of a mitral wave and signs of left ventricular hypertrophy.
Treatment of mitral valve insufficiency, prognosis
Treatment of mitral valve regurgitation is governed by a single rule: a patient diagnosed with mitral regurgitation is a surgical patient. This pathology is not subject to drug correction. The task of the cardiologist is to properly prepare the patient for surgery.
Conservative treatment of mitral valve insufficiency is aimed at controlling the heart rate, as well as preventing thromboembolic complications and reducing the degree of regurgitation. Symptomatic treatment is also used.
During surgery, the mitral valve is implanted.
Prognosis for mitral regurgitation depends entirely on the degree of regurgitation, the severity of the valve defect and the dynamics of the disease.
Video from YouTube on the topic of the article:
The mitral valve exists in every person and is located between the atrium and ventricle of the heart. The condition when there is a gap between the valve leaflets is called mitral valve insufficiency. This disease is dangerous due to its progression and interaction with other defects of the cardiac system.
The causes of this pathology can be both congenital heart disease and untreated infections. Almost always this disease is accompanied by other heart diseases.
Unfortunately, everyone is susceptible to mitral insufficiency, even small children. Let's take a closer look at what mitral valve insufficiency is, the etiology and pathogenesis of the disease, the main symptoms, methods of treatment and prevention.
Mitral valve insufficiency - description
Mitral valve insufficiencyMitral regurgitation is a heart defect in which there is a reverse movement of blood from the left ventricle into the left atrium during contraction of the ventricles of the heart due to incomplete closure of its valves. Mitral regurgitation is the most common type of heart valve disorder.
It is detected in half of patients with heart defects, mainly in combination with mitral stenosis (narrowing of the right atrioventricular orifice) and with aortic defects - stenosis (narrowing of the aorta at the valve level) or aortic valve insufficiency (loose closure of the aortic valves at the time of relaxation of the ventricles ).
Mitral valve insufficiency rarely occurs in isolation (that is, without other heart defects) - only in every fiftieth patient with a heart defect.
The essence of this defect is a violation of the closing function of the valve due to fibrous deformation of the leaflets, subvalvular structures, dilatation of the fibrous ring or disruption of the integrity of the elements of the mitral valve, which causes the return of part of the blood from the left ventricle to the atrium.
These disturbances of intracardiac hemodynamics are accompanied by a decrease in minute volume of blood circulation and the development of pulmonary hypertension syndrome.

The main indicator of mitral valve insufficiency is how much blood there is regurgitation back into the left atrium. Accordingly, degrees of deficiency are distinguished.
- I degree – regurgitation is mild. There is a slight flow of blood into the atrium, which is detected at the valve.
- II degree - the flow of regurgitant blood reaches the middle of the atrium.
- III degree - the blood stream reaches the posterior wall of the atrium. Decompensation of the defect occurs.
This leads to the fact that more blood accumulates in the atrium than it should (that which enters normally + abandoned). This blood enters the ventricle and causes it to contract with greater force than it should.
This leads to ventricular (left) hypertrophy. In this way the defect is compensated.
More blood is thrown back. Now the atrium is no longer able to push out all the blood without a significant fluctuation in pressure. There is an increase in pressure in the left atrium. Accordingly, the pressure in the pulmonary vessels increases.
The left atrium expands because the muscle is no longer able to push out all the blood. In particularly advanced cases, the right ventricle may also increase in size (it is difficult to pump blood to the lungs, where there is stagnation). However, this is quite rare.

All mitral valve insufficiency can be divided into three groups, depending on what is the root cause of the defect.
- Organic failure. In these cases, the cause of insufficiency lies in the valve itself, which is affected by some factor.
In approximately 75% of people, the cause is rheumatism. There are a number of other causes of organic disorders:
- systemic lupus erythematosus - the valve contains a lot of connective tissue, which is affected in an autoimmune disease;
- scleroderma - this disease also refers to connective tissue diseases;
- myxomatous degeneration of the mitral valve - its leaflets are affected, losing the ability to tightly close the atrioventricular opening;
- infective endocarditis - quite often microorganisms affect the valve leaflets;
- mitral valve annulus calcification;
- It is also worth mentioning a number of conditions in which the valve leaflets or chords that give it its shape are torn off.
Mitral valve insufficiency is divided into four degrees according to severity. Stage 1 prolapse is the most light form. In this case, the reverse blood flow is no more than 20% and the entire volume remains within the atrium. Very often this disease is diagnosed together with other heart problems.
Insufficiency of the 1st degree is difficult to diagnose, since it causes almost no visible symptoms, and also allows a person to lead a normal lifestyle. The disease does not prevent pregnancy. All causes that led to the appearance of stage 1 disease are divided into congenital and acquired.
In the first case, the heart defect may be hereditary and occur during fetal development. But most often the disease is acquired (in 99.4% of cases). The causes that led to the development of stage 1 disease are:
- Rheumatism. This damage is expressed as the inability of the immune system to fight certain types of streptococcus. At the same time, rheumatism of the joints and damage to other valves develops.
- Cardiac ischemia. The chordae and papillary muscles responsible for closing the valve become weakened or torn.
- Traumatic injuries. Most often lead to a more pronounced course of the disease.
- Systemic lupus erythematosus. The patient develops damage to connective tissues. Mitral valve insufficiency can be congenital or acquired, including those that are part of the valves.
- Infectious endocarditis. Damage to the mitral valve leaflets by pathogenic microorganisms.
- Scleroderma. Another disease that affects connective tissue cells.
- Myxomatous degeneration of the mitral valve. The valves separating the atrium lose the ability to close tightly, leaving a gap.
- Relative deficiency. The valve is normal, but due to deformation of the left ventricle and stretching of the opening, it loses the ability to close it tightly.
- Functional impairment. Pathologies associated with papillary muscles and myocardium.
The disease occurs in men and women, especially during pregnancy. Most common reason(75% of cases) – infectious disease, pathogenic microorganisms. Timely treatment diseases will be the best prevention of stage 1 deficiency.
Mitral valve insufficiency in children
This condition often occurs in young children and is congenital or acquired. The disease can begin to develop in the baby while still in the womb, which can happen for the following reasons:
- when the expectant mother receives a dose of radiation exposure;
- under the influence of x-ray radiation from the mother;
- in case the mother of the unborn baby carries various infections;
- heredity;
- genetic malformations of the baby in the womb, including those associated with connective tissue problems (Marfan and Ehlers-Danlos syndromes).
The registration of this disease in a child much later than his birth is associated with the influence of the following factors on his body:
- previously experienced heart surgery;
- endocarditis;
- valvulitis;
- heart injuries.
There are such child health problems in which the bicuspid valve undergoes functional failure, in particular:
- tumor formations;
- death or partial deformation of some areas of the heart located near the valve and responsible for its movement;
- rupture of the connective tissue through which the heart muscle contacts the papillary muscles;
- divergence of the valve leaflets due to an increase in the boundaries of the fibrous ring.
Other causes of illness in children may include:
- rheumatism;
- dilated cardiomyopathy;
- systemic lupus erythematosus;
- myocarditis;
- mitral valve prolapse;
- ischemic disease hearts;
- arterial hypertension;
- aortic heart defects.
The congenital variant of the disease develops very rapidly and provokes heart failure in the child. Symptoms in general manifestations are characterized by:
- the child’s inability to engage in prolonged physical activity or exercise;
- weight loss, slow growth;
- appetite disorders;
- pain in the heart and chest;
- the appearance of shortness of breath;
- the presence of a dry cough;
- lethargy;
- tracing heart murmurs;
- formation of the heart hump.
The initial stage of mitral regurgitation in childhood can occur without visible manifestations, making itself felt only during the period of transition to more severe form. Often this condition is accompanied by various heart problems - stenosis, prolapse, and so on.
The clinical picture of the disease varies according to its stage:
- The first is that manifestations of insufficiency are minimal due to the double work of the left parts of the child’s heart.
- The second is that the volume of blood flowing in the opposite direction is 20-40% of the systolic volume. Blood may begin to accumulate in the lungs, forming congestion.
- The third is a more severe form of the disease. About 40-60% of the blood moves in the wrong direction, which provokes the development of heart failure;
- Fourth – regurgitation is more than 60%, the blood flow completely fills the entire left atrium, causing hemodynamic disturbances.
Regurgitation (flow opposite to normal) accounts for up to 20% of the systolic blood volume (this is the name given to the amount of blood that the ventricles of the heart eject in one contraction).
As a result, the baby’s well-being deteriorates, he feels quickly tired, short of breath, and suffers from bouts of dry cough, sometimes with bloody spots in the sputum.
Diagnosis of the disease in childhood is carried out through non-invasive cardiac procedures:
- ultrasound examination;
- electrocardiograms;
- echocardiography;
- spiral computed tomography;
- magnetic resonance imaging;
- radiography.
In private situations, additional diagnostic procedures are required - coronary angiocardiography and catheterization of the cardiac cavities.
The doctor carefully examines the child and evaluates him physical development, skin tone and elasticity, measures pulse and blood pressure. An important part of the examination is listening to heart rhythms, tones and noises, as well as looking for extraneous sounds when the lungs are working.
Percussion of the chest area allows you to clarify the size of the heart, its position and boundaries. Collection and analysis of anamnesis of illness and life involves clarifying complaints, symptoms of the disease, as well as the causative disease. In addition to this, urine and blood tests are prescribed.
Lack of treatment leads to irreversible complications and damage to the child’s internal organs, even death. Since the baby's body is constantly growing, the heart also increases in size, and therefore heart surgery has to be repeated several times. The child is under lifelong observation by a cardiologist and cardiac surgeon.
Since mitral regurgitation often acts as a complication of any causative disease, it is important to eliminate this disease to restore valve function.
The asymptomatic course of the chronic stage of this disease does not require special treatment measures. The remaining stages of the disease involve taking special medications, the tasks of which include:
- maintaining/stabilizing heart rhythms;
- prevention/treatment of circulatory failure.
Conservative therapy does not give the desired effect in the case of late stages of insufficiency, which explains the need for surgical operations (plastic or using a prosthesis).

The main reason for the development of mitral valve insufficiency is rheumatic in nature. In addition, organic mitral insufficiency can occur with infective endocarditis, Libman-Sachs warty endocarditis, with systemic diseases connective tissue.
Functional (relative) mitral regurgitation can occur with sharp dilatation of the left ventricle due to aortic defects (“mitralization” of aortic defects, dilated cardiomyopathy, left ventricular aneurysm, prolapse of the mitral valve leaflets, calcification of the valve ring), disrupting the mechanism of its narrowing during ventricular systole.
The possibility of developing mitral insufficiency after mitral commissurotomy cannot be excluded. According to the flow, it is customary to distinguish between acute and chronic mitral insufficiency.
Acute mitral insufficiency:
- rupture of chordae tendineae as a result of infective endocarditis, myocardial infarction, trauma;
- damage to the papillary muscles;
- valve damage as a complication during cardiac surgery, perforation in infective endocarditis.
Chronic mitral insufficiency:
- rheumatic lesion;
- systemic diseases;
- congenital or hereditary diseases;
- hypertrophic cardiomyopathy;
- mitral valve calcification;
- tumors.
Incomplete closure of the mitral valve leaflets allows blood to flow back (regurgitation) from the ventricle into the atrium during systole. Excessive blood in the left atrium stretches its walls, while increased blood flow into the left ventricle causes it to dilate and then hypertrophy.
Subsequently, with weakening of the left atrium and under the influence of regurgitation waves, the atrial myocardium loses its tone, the pressure in the cavity of the left atrium increases, which is retrogradely transmitted to the pulmonary veins - venous pulmonary hypertension, which ends with progressive right ventricular decompensation.
Features of hemodynamics in mitral insufficiency:
- regurgitation up to 5 ml has no practical significance;
- clinical manifestations - with regurgitation in the left atrium of at least 10 ml;
- long-term compensation of the defect (provided by the hypertrophied left ventricle according to the Frank-Starling mechanism);
- rapid progression with decompensation.
An increase in stroke and cardiac output, a decrease in end-systolic volume and the absence of pulmonary hypertension are indicators of a compensated hemodynamic state.

This defect is quite successfully compensated by the internal reserves of the body (primarily the heart). Therefore, patients experience any discomfort for a long time and do not turn to doctors for help. However, a number of more or less specific symptoms can be noted.
- A cough, initially dry, then with the addition of sputum streaked with blood, appears as the severity of blood stagnation in the vessels of the lungs increases.
- Shortness of breath - occurs as a result of stagnation of blood in the vessels of the lungs.
- Rapid heartbeat, a feeling of irregular heartbeat, cardiac arrest, upheavals in the left half of the chest - occurs with the development of arrhythmias (heart rhythm disturbances) due to damage to the heart muscle by the same process that caused mitral valve insufficiency (for example, heart injury or myocarditis - inflammation of the heart muscle ) and due to changes in the structure of the atrium.
- General weakness and decreased performance are associated with impaired blood distribution in the body.
However, all these symptoms can also appear in other heart defects and diseases, so the clinical picture cannot be the basis for making a diagnosis; a number of studies are being carried out.
Clinically, in the stage of compensation of the defect, patients feel satisfactory, can perform significant physical activity, the pathology is detected by chance.
In the future, with a decrease in the contractile function of the left. ventricle and increased pressure in the pulmonary circulation, patients complain of shortness of breath during exercise and palpitations. Attacks of cardiac asthma and shortness of breath at rest may occur.
A cough may occur, and rarely, hemoptysis. Cardialgia is observed - stabbing, aching, pressing, without a clear connection with physical activity. Left ventricular failure may be joined by right ventricular failure (swelling, pain in the right hypochondrium due to liver enlargement and capsule stretching), and later - total decompensation.
During physical examination, attention is drawn to acrocyanosis and fades mitralis, sometimes “heart hump”. On palpation, an intensified diffuse apical impulse is found, caused by hypertrophy and dilatation of the left ventricle, localized in the fifth intercostal space outward from the midclavicular line or in the sixth intercostal space (more often in young patients).
The boundaries of relative cardiac dullness are expanded to the left, up and to the right. Auscultation of the heart: the first sound is weakened at the apex (up to its complete absence) - since there is no “period of valve closure,” vibrations caused by a wave of regurgitation can be layered.
An increased pathological third heart sound is often heard, caused by vibrations of the walls of the left ventricle. The tone has main differences: dull in timbre, audible in a limited area.
The decisive sign of the defect is a systolic murmur - soft, blowing, decreasing, ending before the second sound appears, spreading to the axillary region, auscultated as much as possible during a deep breath with the patient lying on his left side. The louder and longer the systolic murmur, the more severe the mitral regurgitation.
Above the pulmonary artery there is an accent of the second tone, moderately expressed and associated with the development of congestion in the pulmonary circle. Often a splitting of the second tone is heard, associated with a delay in the aortic component of the tone, since the period of expulsion of an increased amount of blood from the left ventricle becomes longer.
When examining the lungs, signs are found indicating congestion in the pulmonary circulation (weakening of breathing, shortening of percussion sound, crepitus or fine, silent, moist rales in the posterior lower parts of the lungs).
Subsequent weakening of the right ventricle leads to stagnation of blood in the systemic circulation, which is clinically manifested by an enlarged liver and edema of the lower extremities. In the later stages, congestive cirrhosis of the liver and ascites develop.
With a compensated defect, the pulse and blood pressure remain normal; with decompensation, the pulse increases and blood pressure may decrease slightly. In later stages, atrial fibrillation is often observed.

Already during a routine examination one can suspect a change in the mitral valve:
- the patient’s characteristic complaints allow us to assess the degree of heart failure;
- murmurs are detected on auscultation;
- upon percussion, the boundaries of cardiac dullness shift to left side.
Main diagnostic meaningful method for mitral regurgitation, ultrasound of the heart is used, which can be supplemented with Doppler ultrasound, which allows a more visual assessment of the degree of regurgitation.
With ECHO-CG it is possible to determine the cause of the heart defect, as well as complications of this condition. Based on the measurements obtained, the degree of deficiency can be judged.
It should be noted that isolated mitral valve disease is quite rare and in most cases is caused by rheumatic changes.
Much more often, ultrasound of the heart reveals combined insufficiency of the mitral and tricuspid valves. Such changes quickly lead to decompensation of heart failure and require prompt medical intervention.
Auxiliary diagnostic methods are:
- ECG, which changes only with secondary transformation of the heart muscle.
- X-ray of the chest, in which one can suspect a general increase in size of the heart.
- Transesophageal ECG helps diagnose atrial rhythm disturbances.
- Daily monitoring is performed for paroxysmal arrhythmias.
- Phonocardiography can detect murmur.
- With ventriculography using special contrast, the degree of regurgitation can be more accurately determined.
- Coronary angiography is performed as preoperative preparation or if the ischemic nature of the defect is suspected.
- Analysis of the medical history and complaints - how long ago shortness of breath, palpitations, cough (initially dry, then with sputum mixed with blood) appeared, what the patient associates with their occurrence.
- Life history analysis. It turns out what the patient and his close relatives were sick with, who the patient is by profession (whether he had contact with pathogens infectious diseases), whether there were any infectious diseases.
- Physical examination. On examination, cyanosis (blueness) of the skin, “mitral blush” (bright red coloring of the patient’s cheeks due to impaired oxygenation of the blood), “heart hump” is noted - this is a pulsating protrusion to the left of the sternum (the central bone of the chest to which the ribs are attached) behind due to a significant increase in the left ventricle of the heart.
- Blood and urine analysis. It is carried out to identify the inflammatory process and concomitant diseases.
- Blood chemistry. The level of cholesterol (a fat-like substance), sugar and total blood protein, creatinine (a protein breakdown product), uric acid (a breakdown product of purines - substances from the cell nucleus) is determined to identify concomitant organ damage.
- Immunological blood test. The content of antibodies to various microorganisms and the heart muscle (special proteins produced by the body that can destroy foreign substances or cells of the body’s own) and the level of C-reactive protein (a protein whose level increases in the blood during any inflammation) will be determined.
- Electrocardiographic study (ECG) - allows you to evaluate the rhythm of heartbeats and the presence of disorders heart rate(for example, premature contractions of the heart), the size of the parts of the heart and its overload.
- A phonocardiogram (a method for analyzing heart sounds) with mitral valve insufficiency demonstrates the presence of systolic (that is, during contraction of the ventricles of the heart) noise in the projection of the bicuspid valve.
- Echocardiography (EchoCG - ultrasound examination of the heart) is the main method for determining the condition of the mitral valve.
- X-ray of the chest organs - evaluates the size and location of the heart, changes in the configuration of the heart (protrusion of the shadow of the heart in the projection of the left atrium and left ventricle), the appearance of blood stagnation in the vessels of the lungs.
- Catheterization of the cardiac cavities is a diagnostic method based on inserting catheters (medical instruments in the form of a tube) into the cardiac cavities and measuring the pressure in the left atrium and left ventricle.
- Spiral CT scan(SCT), a method based on taking a series of X-rays at different depths, and magnetic resonance imaging (MRI), a method based on building chains of water when strong magnets are applied to the human body, allow you to obtain an accurate image of the heart.
- Coronary cardiography (CCG) is a method in which contrast (a dye) is injected into the own vessels of the heart and the heart cavity, which makes it possible to obtain an accurate image of them, as well as to evaluate the movement of blood flow.
The history may indicate a rheumatic process, inflammatory diseases, chest injuries, tumors.
Percussion (tapping) reveals expansion of the heart to the left. Auscultation (listening) of the heart reveals a murmur during systole (the period of contraction of the ventricles of the heart) in the region of the apex of the heart.
Mitral valve insufficiency is most characterized by an ECG showing an enlargement of the left atrium and left ventricle.
The area of the left atrioventricular orifice is measured, the mitral valve leaflets are examined for changes in their shape (for example, wrinkling of the leaflets or the presence of ruptures in them), loose closure during contraction of the ventricles of the heart, and the presence of vegetations (additional structures on the valve leaflets).
EchoCG also evaluates the size of the heart cavities and the thickness of its walls, the condition of other heart valves, thickening of the endocardium (the inner lining of the heart), and the presence of fluid in the pericardium (the sac around the heart).
Doppler echocardiography (ultrasound examination of the movement of blood through the vessels and chambers of the heart) reveals the reverse flow of blood from the left ventricle into the left atrium during ventricular contraction, as well as an increase in pressure in pulmonary arteries(vessels that bring blood to the lungs).
With mitral valve insufficiency, the pressure in the left atrium becomes almost the same as in the left ventricle.
It is carried out when planning surgical treatment of a defect or suspected concomitant coronary heart disease.
Treatment of mitral regurgitation
Mild disease, which is not accompanied by symptoms, special treatment does not require.
Moderate mitral valve insufficiency is not an indication for surgery. In this case, treatment is carried out with the help of medications:
- ACE inhibitors prevent secondary transformation of the heart myocardium and reduce symptoms of heart failure;
- beta blockers reduce the frequency of contractions of the left ventricle, thereby increasing the ejection fraction;
- diuretics accelerate the removal of fluid from the body and eliminate symptoms of stagnation;
- Vasodilators reduce the load on the heart by depositing blood and fluid in the peripheral arteries;
- cardiac glycosides stimulate heart contractions and help fight arrhythmia;
- It makes sense to use anticoagulants for persistent atrial fibrillation;
- antibiotics are prescribed for infective endocarditis;
- Hormonal medications can affect the course of rheumatism.
In case of acute development of regurgitation, intra-aortic balloon counterpulsation can be used. During this procedure, a special oval inflating balloon is inserted into the patient's aorta, which opens in opposition to the contractions of the heart.
As a result, coronary blood flow increases and the ejection fraction also increases. This measure is temporary and is mainly suitable for ischemia of the papillary muscles, or as preoperative preparation.
- It is necessary to treat the underlying disease - the cause of mitral valve insufficiency.
- Drug treatment is indicated for complications of mitral regurgitation (for example, treatment of heart failure, cardiac arrhythmias, etc.)
- Mild or moderate mitral valve insufficiency does not require special treatment.
In case of pronounced and severe mitral insufficiency, surgery: plastic or replacement of the mitral valve.
- Surgical treatment of tricuspid valve insufficiency is carried out exclusively under artificial circulation (during the operation, blood throughout the body is pumped not by the heart, but by an electric pump).
Types of operations:
- Plastic surgery (that is, normalization of blood flow through the left atrioventricular orifice while preserving the native mitral valve) is performed in case of mitral valve insufficiency of 2-3 degrees and the absence of pronounced changes in its leaflets.
- Ring annuloplasty (valve surgery) by sewing in a support ring at the base of the mitral valve leaflets. The ring consists of a metal base covered with synthetic fabric;
- Shortening of the chordae (tendon strands that attach the papillary muscles to the heart muscle - the internal muscles of the heart that ensure the movement of the valves);
- Removal of part of the elongated posterior mitral valve leaflet.
- biological prostheses (made from the aorta (that is, the largest vessel) of animals) - used in children and women who are planning a pregnancy;
- mechanical valves (made from special medical metal alloys) are used in all other cases.
- After implantation of a mechanical prosthesis, patients need to constantly take drugs from the group of indirect anticoagulants (drugs that reduce blood clotting by blocking the liver's synthesis of substances necessary for clotting).
- After implantation of a biological prosthesis, anticoagulant therapy is carried out for a short period of time (1-3 months).
- After valve repair, anticoagulant therapy is not performed.

Along with the treatment of the underlying disease at stages 1 and 2 of insufficiency, supportive and corrective symptomatic drug treatment is carried out:
- The use of vasodilators to regulate systolic pressure in the aorta and the effect of ACE inhibitors in this case are considered the most studied;
- Adrenergic blockers;
- The use of anticoagulants to avoid thrombosis;
- Diuretics and antioxidants;
- Antibiotics as a preventative measure, especially for prolapse.
It should be noted that drug treatment is futile and the patient’s condition should not be allowed to deteriorate to such an extent that irreversible consequences in the heart will reduce the prognosis for successful surgery or make the operation impossible, since the more complex the operation, the higher the mortality rate.
With the help of medications, the patient’s condition can be stabilized, but even with medications, the disease often progresses.
Surgery for illness

It is impossible to completely cure mitral valve defects with medication, especially at the border of stages 2, 3 and 4.
If the disease progresses or acute failure occurs, and there is no compelling reason to cancel the operation, surgery is the only effective method of treatment.
During the operation, plastic surgery or prosthetics of the required areas is performed, and the patient is connected to the artificial circulation system during the operation.
Plastic surgery is used when there are no pronounced changes in the structure of the mitral valve leaflets. Depending on the pathology (prolapse, “threshing” valve, etc.) the following is carried out:
- Correction of valve leaflet size;
- Shortening of tendon threads (regulation of valve movement);
- The size of the mitral ring is corrected; a special ring is sewn in at the base of its valves (annuloplasty).
Commissurotomy (expansion of the lumen of the mitral valve) can be performed transthoracically, without connecting to a heart-lung machine. In case of calcification and low mobility of the valve, a full-fledged operation is performed with the connection of artificial circulation.
Commissurotomy can eliminate serious defects, but after such an operation stenosis may subsequently develop.
Valvuloplasty is aimed at restoring a narrowed valve.
Balloon valvuloplasty does not require disconnecting the heart from the circulatory system; the operation is performed through an incision in the artery or vein of the thigh. This is the safest operation with the minimum number of complications.
Valve-sparing reconstructive surgeries in children, such as leaflet decalcification and commissuroplasty, have a favorable prognosis. But in three out of ten cases, you have to do a second operation to replace the mitral valve.
To avoid this, in the preoperative period the degree of regurgitation is measured, the exact parameters of the mitral valve and mitral ring are determined, the indicators are compared with the parameters of the child’s body, and a tentative prognosis is calculated according to which it is either advisable to perform reconstructive surgery or immediately perform mitral valve replacement.
Mitral valve replacement is used in cases of severe changes in the valve or when repair has failed. For children, biological prostheses made from animal aorta are used, which, as a rule, take root well.
The operation allows you to eliminate almost any defects, does not subsequently cause the development of stenosis, and after six months postoperative period the child will be able to lead a full life.

To prevent the disease, annual examinations are carried out. If the disease is asymptomatic, then the only preventive measure is an annual cardiac ultrasound procedure. It is necessary in order to prevent and identify in advance any changes in the functioning of the heart.
Preventive measures are also prescribed in case of secondary occurrence of the defect. In this case, all measures are aimed at eliminating foci of chronic infection that led to failure. Additionally, signs of hypercholesterolemia are eliminated. The patient should undergo regular diagnostic testing and visit the doctor.
If you follow all the doctor’s recommendations, and also if you adhere to healthy image life, then mitral valve problems may not manifest themselves throughout life. This disease does not greatly affect a person’s performance and has no contraindications.
Mitral valve insufficiency of the 1st degree is a minor form of the disease. Difficult to diagnose. Does not require surgery.
Treatment of any heart failure is mandatory; without timely treatment, congestion in organs and irreversible complications develop varying degrees, but even with deterrent drug treatment, mortality remains high.
Naturally, any heart surgery is a risk; mortality after open heart surgery is 1–3% for children and increases with the number of concomitant diseases.
Valvuloplasty and camisurotomy are temporary measures; treatment of insufficiency with these methods is impossible and over time the procedures will have to be repeated periodically. After prosthetics, the patient receives postoperative treatment and is under the supervision of a doctor for life.
During the appointment, a mandatory auscultation of the child’s heart is performed; other studies are prescribed as needed.
Source » hospital-israel.ru; lookmedbook.ru; pirogov-center.ru; iserdce.ru; mirbodrosti.com; detstrana.ru; bone-surgery.ru; lecheniedetej.ru"
serdtse1.ru
Description of the disease
MVR (mitral valve insufficiency) is the most common cardiac anomaly. Of all the sick 70% suffer from an isolated form of cerebrovascular accident. Typically, rheumatic endocarditis is the main underlying cause of the disease. Often, a year after the first attack, the heart condition leads to chronic failure, the cure of which is quite difficult.
The highest risk group includes people with valvulitis.. This disease damages the valve leaflets, as a result of which they undergo processes of wrinkling, destruction, and gradually become shorter than their original length. If valvulitis is at an advanced stage, calcification develops.
Septic endocarditis leads to the destruction of many cardiac structures, so NMC has the most strong manifestations. The valve flaps do not fit together tightly enough. When they are not completely closed through the valve, too much blood coming out, which provokes its reboot and the formation of stagnant processes, an increase in pressure. All signs lead to increasing insufficiency of uric acid.
Causes and risk factors
NMC affects people with one or more of the following pathologies:

- Congenital predisposition.
- Connective tissue dysplasia syndrome.
- Mitral valve prolapse, characterized by regurgitation of 2 and 3 degrees.
- Destruction and breakage of the chords, rupture of the valves of the mitral valve due to injuries in the chest area.
- Rupture of the valves and chords with the development of infectious endocarditis.
- Destruction of the apparatus connecting the valves in endocarditis resulting from connective tissue diseases.
- Infarction of part of the mitral valve with subsequent scar formation in the subvalvular region.
- Changes in the shape of the valves and tissues located under the valves when rheumatism.
- Enlargement of the mitral annulus during dilatation cardiomyopathy.
- Insufficiency of valve function in the development of hypertrophic cardiomyopathy.
- MK insufficiency due to surgery.
Mitral regurgitation is often accompanied by another defect - mitral valve stenosis.
Types, forms, stages
With NMC the total stroke volume of the left ventricle is estimated. Depending on its quantity, the disease is divided into 4 degrees of severity (the percentage indicates the part of the blood that is redistributed incorrectly):
- I (the softest) - up to 20%.
- II (moderate) - 20-40%.
- III (medium form) - 40-60%.
- IV (heaviest) - over 60%.
According to the forms of its course, the disease can be divided into acute and chronic:

When determining the features of movement of the mitral valves, there are 3 types of pathology classification:
- 1 - standard level of mobility of the leaflets (in this case, painful manifestations consist of dilatation of the fibrous ring, perforation of the leaflets).
- 2 - destruction of the valves (the chords take the greatest damage, as they are stretched or ruptured, and a violation of the integrity of the papillary muscles also occurs.
- 3 - decreased mobility of the valves (forced connection of commissures, reduction in the length of the chords, as well as their fusion).
Danger and complications
With the gradual progression of NMC, the following disorders appear:
- The development of thromboembolism due to constant stagnation of a large part of the blood.
- Valve thrombosis.
- Stroke. Previously occurring valve thrombosis is of great importance in the risk factors for stroke.
- Atrial fibrillation.
- Symptoms of chronic heart failure.
- Mitral regurgitation (partial failure of the mitral valve to perform functions).
Symptoms and signs
The severity and severity of MCT depends on the degree of its development in the body:
- Stage 1 the disease has no specific symptoms.
- Stage 2 does not allow patients to carry out physical activity in an accelerated mode, since shortness of breath, tachycardia, pain in the chest, loss of heart rhythm, and discomfort immediately appear. Auscultation with mitral insufficiency determines increased tone intensity and the presence of background noise.
- Stage 3 characterized by left ventricular failure and hemodynamic pathologies. Patients suffer from constant shortness of breath, orthopnea, accelerated heart rate, feel discomfort in the chest, their skin paler than in a healthy state.
Find out more about mitral regurgitation and hemodynamics with it from the video:
When to see a doctor and which one
When identifying symptoms characteristic of MCT, it is necessary contact a cardiologist immediately, to stop the disease in its early stages. In this case, you can avoid the need to consult with other doctors.
Sometimes there is suspicion of a rheumatoid etiology of the disease. Then you should visit a rheumatologist for diagnosis and proper treatment. If there is a need for surgical intervention, treatment and subsequent the problem is resolved by a cardiac surgeon.
Common methods for detecting NMC:

Learn more about symptoms and diagnosis from the video:
It is necessary to distinguish NMC from other heart pathologies:
- Myocarditis in severe form.
- Congenital and acquired heart defects of related etiology.
- Cardiomyopathies.
- MK prolapse.
Therapy methods
If symptoms of cervical urinary tract are severe, surgical intervention is indicated for the patient. The operation is performed urgently for the following reasons:

- In the second and later stages, despite the fact that the volume of blood ejected is 40% of its total amount.
- If there is no effect from antibacterial therapy and aggravation of infectious endocarditis.
- Increased deformation, sclerosis of the valves and tissues located in the subvalvular space.
- In the presence of signs of progressive left ventricular dysfunction together with general heart failure occurring at 3-4 degrees.
- Heart failure in the early stages can also be a reason for surgery, however, to form an indication, thromboembolism of large vessels located in the systemic circulation must be detected.
The following operations are practiced:
- Valve-sparing reconstructive surgeries are necessary to correct cerebrovascular accidents in childhood.
- Commissuroplasty and decalcification of the leaflets are indicated for severe MV insufficiency.
- Chordoplasty is intended to normalize the mobility of the valves.
- Translocation of cords is indicated when they fall off.
- Fixation of parts of the papillary muscle is carried out using Teflon gaskets. This is necessary when separating the head of the muscle from the remaining components.
- Prosthetics of the chords is necessary when they are completely destroyed.
- Valvuloplasty avoids leaflet rigidity.
- Anuloplasty is intended to relieve the patient of regurgitation.
- Valve replacement is carried out when it is severely deformed or when fibrosclerosis develops irreparably and interferes with normal functioning. Mechanical and biological prostheses are used.
Learn about minimally invasive operations for this disease from the video:
What to expect and preventive measures
With the development of cerebrovascular accident, the prognosis determines the severity of the disease, that is, the level of regurgitation, the occurrence of complications and irreversible changes in cardiac structures. Survival rate 10 years after diagnosis is higher than for similar severe pathologies.
If valve insufficiency is mild or moderate, women have the ability to bear and give birth to children. When the disease becomes chronic, all patients should undergo an annual ultrasound and visit a cardiologist. If worsening occurs, you should visit the hospital more often.
Prevention of NMC consists in preventing or promptly treating diseases that cause this pathology. All diseases or manifestations of mitral valve insufficiency due to an abnormal or reduced valve must be quickly diagnosed and promptly treated.
NMC is a dangerous pathology that leads to severe destructive processes in the heart tissue, and therefore requires proper treatment. Patients, if they follow the doctor’s recommendations, may, some time after starting treatment,
The pathology is characterized by regurgitation of blood into the left atrium from the left ventricle. Let us consider in detail what it is, the nature of development and clinical picture the course of mitral valve insufficiency in degrees 1, 2 and 3 of the disease, methods of its treatment and prognosis for returning to normal life.
Description of the disease
MVR (mitral valve insufficiency) is the most common cardiac anomaly. Of all patients, 70% suffer from an isolated form of cerebrovascular accident. Typically, rheumatic endocarditis is the main underlying cause of the disease. Often, a year after the first attack, the heart condition leads to chronic failure, the cure of which is quite difficult.
The highest risk group includes people with valvulitis. This disease damages the valve leaflets, as a result of which they undergo processes of wrinkling, destruction, and gradually become shorter than their original length. If valvulitis is at an advanced stage, calcification develops.
Septic endocarditis leads to the destruction of many cardiac structures, so NMC has the most severe manifestations. The valve flaps do not fit together tightly enough. When they are not completely closed, too much blood comes out through the valve, which provokes its reboot and the formation of stagnant processes, an increase in pressure. All signs lead to increasing insufficiency of uric acid.
Causes and risk factors
NMC affects people with one or more of the following pathologies:
- Congenital predisposition.
- Connective tissue dysplasia syndrome.
- Mitral valve prolapse, characterized by regurgitation of 2 and 3 degrees.
- Destruction and breakage of the chords, rupture of the valves of the mitral valve due to injuries in the chest area.
- Rupture of the valves and chords with the development of infectious endocarditis.
- Destruction of the apparatus connecting the valves in endocarditis resulting from connective tissue diseases.
- Infarction of part of the mitral valve with subsequent scar formation in the subvalvular region.
- Changes in the shape of the valves and tissues under the valves in rheumatism.
- Enlarged mitral annulus in dilated cardiomyopathy.
- Insufficiency of valve function in the development of hypertrophic cardiomyopathy.
- MK insufficiency due to surgery.
Mitral regurgitation is often accompanied by another defect - mitral valve stenosis.
Types, forms, stages
With NMC, the total stroke volume of the blood of the left ventricle is assessed. Depending on its quantity, the disease is divided into 4 degrees of severity (the percentage indicates the part of the blood that is redistributed incorrectly):
- I (the softest) - up to 20%.
- II (moderate) -%.
- III (medium form) -%.
- IV (heaviest) - over 60%.
According to the forms of its course, the disease can be divided into acute and chronic:
When determining the characteristics of the movement of the mitral leaflets, 3 types of pathology classification are distinguished:
- 1 - standard level of mobility of the leaflets (in this case, painful manifestations consist of dilatation of the fibrous ring, perforation of the leaflets).
- 2 - destruction of the valves (the chords take the greatest damage, as they are stretched or ruptured, and a violation of the integrity of the papillary muscles also occurs.
- 3 - decreased mobility of the valves (forced connection of commissures, reduction in the length of the chords, as well as their fusion).
Danger and complications
With the gradual progression of NMC, the following disorders appear:
- The development of thromboembolism due to constant stagnation of a large part of the blood.
- Valve thrombosis.
- Stroke. Previously occurring valve thrombosis is of great importance in the risk factors for stroke.
- Atrial fibrillation.
- Symptoms of chronic heart failure.
- Mitral regurgitation (partial failure of the mitral valve to perform functions).
Symptoms and signs
The severity and severity of MCT depends on the degree of its development in the body:
- Stage 1 of the disease has no specific symptoms.
- Stage 2 does not allow patients to carry out physical activity in an accelerated manner, since shortness of breath, tachycardia, pain in the chest, loss of heart rhythm, and discomfort immediately appear. Auscultation with mitral insufficiency determines increased tone intensity and the presence of background noise.
- Stage 3 is characterized by left ventricular failure and hemodynamic pathologies. Patients suffer from constant shortness of breath, orthopnea, increased heart rate, chest discomfort, and their skin is paler than in a healthy state.
Find out more about mitral regurgitation and hemodynamics with it from the video:
When to see a doctor and which one
If you identify symptoms characteristic of MCT, you must immediately contact a cardiologist to stop the disease in the early stages. In this case, you can avoid the need to consult with other doctors.
Sometimes there is suspicion of a rheumatoid etiology of the disease. Then you should visit a rheumatologist for diagnosis and proper treatment. If there is a need for surgical intervention, treatment and subsequent elimination of the problem is carried out by a cardiac surgeon.
Diagnostics
Common methods for detecting NMC:
- Physical. The speed and uniformity of the pulse, features of changes are assessed blood pressure, severity of systolic murmurs in the lungs.
During the examination, doctors pay attention to the patient’s breathing pattern. During the disease, shortness of breath does not stop even when the patient moves to a horizontal position, and manifests itself when distractions, physical and mental stimuli are excluded. On examination there is a pasty appearance feet and legs, decreased diuresis.
Learn more about symptoms and diagnosis from the video:
It is necessary to distinguish NMC from other heart pathologies:
- Myocarditis in severe form.
- Congenital and acquired heart defects of related etiology.
- Cardiomyopathies.
- MK prolapse.
You can read about the symptoms of aortic valve insufficiency and the differences between this heart defect and the one described in this article in another material.
Also read the information about how Behcet's disease appears and how dangerous it is, with methods for treating this complex vascular pathology.
Therapy methods
If symptoms of cervical urinary tract are severe, surgical intervention is indicated for the patient. The operation is performed urgently for the following reasons:
- In the second and later stages, despite the fact that the volume of blood ejected is 40% of its total amount.
- In the absence of effect from antibacterial therapy and worsening of infectious endocarditis.
- Increased deformation, sclerosis of the valves and tissues located in the subvalvular space.
- In the presence of signs of progressive left ventricular dysfunction together with general heart failure occurring at 3-4 degrees.
- Heart failure in the early stages can also be a reason for surgery, however, to form an indication, thromboembolism of large vessels located in the systemic circulation must be detected.
The following operations are practiced:
- Valve-sparing reconstructive surgeries are necessary to correct cerebrovascular accidents in childhood.
- Commissuroplasty and decalcification of the leaflets are indicated for severe MV insufficiency.
- Chordoplasty is intended to normalize the mobility of the valves.
- Translocation of cords is indicated when they fall off.
- Fixation of parts of the papillary muscle is carried out using Teflon gaskets. This is necessary when separating the head of the muscle from the remaining components.
- Prosthetics of the chords is necessary when they are completely destroyed.
- Valvuloplasty avoids leaflet rigidity.
- Anuloplasty is intended to relieve the patient of regurgitation.
- Valve replacement is carried out when it is severely deformed or when fibrosclerosis develops irreparably and interferes with normal functioning. Mechanical and biological prostheses are used.
Learn about minimally invasive operations for this disease from the video:
What to expect and preventive measures
With the development of cerebrovascular accident, the prognosis determines the severity of the disease, that is, the level of regurgitation, the occurrence of complications and irreversible changes in cardiac structures. Survival rate 10 years after diagnosis is higher than for similar severe pathologies.
If valve insufficiency manifests itself in moderate or moderate form, women are able to bear and give birth to children. When the disease becomes chronic, all patients should undergo an annual ultrasound and visit a cardiologist. If worsening occurs, you should visit the hospital more often.
Prevention of NMC consists of preventing or promptly treating the diseases that cause this pathology. All diseases or manifestations of mitral valve insufficiency due to an abnormal or reduced valve must be quickly diagnosed and promptly treated.
NMC is a dangerous pathology that leads to severe destructive processes in the heart tissue, and therefore requires proper treatment. Patients, if they follow the doctor’s recommendations, can return to normal life and cure the disorder some time after starting treatment.
Overview of mitral regurgitation, 1, 2 and other degrees of the disease
From this article you will learn: what mitral valve insufficiency is, why it develops, and how it manifests itself. Degrees of the disease and their characteristics. How to get rid of mitral valve insufficiency.
Mitral valve insufficiency is a defect in which its leaflets are unable to close completely. Because of this, regurgitation (backflow of blood) from the left ventricle into the left atrium occurs.
The disease is dangerous because it leads to heart failure, circulatory disorders and related disorders of internal organs.
Valve disease can be completely cured with surgery. Conservative treatment is more symptomatic.
Treatment is provided by a cardiologist, cardiac surgeon, and rheumatologist.
Causes
This is an acquired defect, not congenital. Its causes can be diseases that damage the connective tissues of the body (since valves are made of connective tissue), heart disease and abnormalities of the valve itself.
Possible causes of mitral valve disease:
Symptoms, degrees and stages
The disease can occur in acute and chronic forms.
Acute mitral regurgitation occurs when the chordae tendineae or papillary muscles rupture during a heart attack or during infective endocarditis, as well as during cardiac injury.
Chronic develops gradually (in 5 stages) due to chronic diseases, such as rheumatism, systemic lupus erythematosus, coronary heart disease, as well as due to pathologies of the mitral valve itself (its prolapse, degeneration).
Symptoms of acute bicuspid valve insufficiency:
- A sharp drop in blood pressure leading to cardiogenic shock.
- Left ventricular failure.
- Pulmonary edema (manifested by suffocation, coughing, wheezing, sputum production).
- Atrial extrasystoles.
- Atrial fibrillation.
Degrees of mitral regurgitation
The severity of the defect can be determined by echocardiography (ultrasound of the heart). It depends on the volume of blood that flows back into the left atrium and the size of the hole that remains when the valve leaflets close.
Characteristics of degrees of severity:
Stages of the disease: characteristics and symptoms
Depending on the severity of the defect, the severity of circulatory disorders and the symptoms that bother the patient, 5 stages are distinguished:
- Compensation stage. It is characterized by grade 1 mitral valve insufficiency (regurgitation volume less than 30 ml). There are no circulatory disorders in the small and large circles. The patient is not bothered by any symptoms. The disease can be detected by chance during a routine medical examination.
- Subcompensation stage. The severity according to echocardiography is moderate. The reverse flow of blood into the left atrium leads to its expansion (dilatation). To compensate for circulatory disorders, the left ventricle is forced to contract more intensely, which leads to its increase - hypertrophy. With intense physical activity, shortness of breath and increased heart rate appear, which indicates that there is still a slight disturbance of blood circulation in the pulmonary (small) circle. Slight swelling of the legs (feet and legs) is possible.
- Stage of decompensation. The severity of regurgitation is 2–3. At this stage, blood circulation is disrupted in both the small and large circles. This is expressed by shortness of breath during any physical exertion, significant enlargement of the left ventricle, pressing, aching or stabbing pain in the left half of the chest (usually after physical activity), periodic heart rhythm disturbances.
- Dystrophic stage. Degree of severity – third (regurgitation more than 60 ml or 50%). The functioning of not only the left, but also the right ventricle is impaired. Echocardiography or chest x-ray may reveal hypertrophy of both ventricles. Blood circulation in both circles is significantly worsened. Because of this, severe swelling appears in the legs, pain both on the left and in the right hypochondrium (can also occur at rest), shortness of breath after minor physical activity or at rest, attacks of cardiac asthma (choking, coughing). Kidney and liver disorders appear. At this stage, tricuspid valve insufficiency may also be added to mitral valve insufficiency.
- Terminal stage. Corresponds to stage 3 of chronic heart failure. The functioning of all parts of the heart is impaired. The heart is no longer able to properly supply blood to all organs. The patient is concerned about shortness of breath at rest, frequent attacks of cardiac asthma, interruptions in heart function, intolerance to any physical activity, swelling of the limbs and abdomen, pain in the heart, arrhythmias (atrial fibrillation, atrial extrasystoles). Irreversible dystrophic changes in internal organs(primarily the kidneys and liver). The prognosis is extremely unfavorable. Treatment is no longer effective.
Diagnostics
To identify the disease, one or more procedures are used:
- conventional echocardiography;
- transesophageal echocardiography;
- X-ray of the chest organs;
Treatment
It can be surgical or medical. However, drug treatment cannot completely eliminate the pathology. Mitral regurgitation can only be completely cured through surgery.
Treatment tactics
At acute form For mitral regurgitation, medications are urgently administered to relieve symptoms, and then surgery is performed.
In the chronic form, treatment tactics depend on the stage.
Drug treatment
In the acute form of the disease, nitrates (Nitroglycerin) and non-glycoside inotropic drugs (for example, Dobutamine) are administered to the patient as first aid. After this, emergency surgery is performed.
In the chronic form, treatment should be aimed both at improving the functioning of the heart and blood circulation, and at getting rid of the underlying disease.
To correct circulatory disorders, diuretics, beta-blockers, aldosterone antagonists, nitrates, antiarrhythmic drugs, and ACE inhibitors are used. If the risk of thrombosis is increased, antiplatelet agents are used.
Treatment of the underlying disease that caused the mitral valve pathology:
Surgery
It is prescribed for the acute form of the disease, as well as for the second and higher stages of the chronic form.
In modern surgical practice, two types of operations are used:
- Valve plastic surgery. This is the reconstruction of your own valve (suturing its valves and chordae tendineae).
- Valve replacement. This is its replacement with a prosthesis of artificial or biological origin.
By performing the operation on time, you can prevent further progression of the defect and associated heart failure.
Prevention
Preventive measures consist of treating the underlying disease even before the onset of mitral regurgitation (timely treatment of endocarditis with antibiotics, correct technique medications prescribed by a doctor for rheumatism, etc.).
Eliminate factors that increase the risk of heart disease: smoking, alcoholism, frequent consumption of fatty, salty and spicy foods, improper drinking regimen, lack of sleep, low mobility, obesity, stress, poor distribution of work and rest time.
Living with mitral regurgitation
If the defect is of the first degree of severity and is in the stage of compensation, you can only get by with observation from a doctor and taking a minimum amount of medication. Visit a cardiologist and do an echocardiogram every six months.
Physical activity within reasonable limits is not contraindicated, however, competitive sports activities are excluded at any stage of the disease.
As for pregnancy, early stage defect without pronounced circulatory disorders, it is possible, but childbirth will take place through caesarean section. For stage 2 or higher disease, successful pregnancy is possible only after the defect is eliminated.
After valve replacement, follow healthy lifestyle rules to prevent cardiovascular diseases. If you need any operations (including dental) or invasive diagnostic procedures in the future, notify your doctor in advance about the presence of a prosthetic valve, as you will be prescribed special medications to prevent inflammation and blood clots in the heart.
Forecast
The prognosis depends on the cause of the defect.
- In most cases, it is unfavorable, since the underlying diseases (rheumatism, lupus, Marfan syndrome, coronary heart disease) are difficult to treat and cannot be completely stopped. Thus, the disease can lead to other damage to the heart, blood vessels and internal organs.
- If the defect was caused by endocarditis or degenerative changes in the valve itself, the prognosis is more comforting. Cure is possible if timely surgery for plastic surgery or valve replacement is performed. The installed prosthesis will last from 8 to 20 years or more, depending on the type.
- The prognosis for a defect of 1st degree of severity, which is not accompanied by circulatory disorders, can be favorable. With proper monitoring tactics, as well as treatment of the underlying disease, mitral regurgitation may not progress for many years.
Treatment of the heart and blood vessels © 2016 | Sitemap | Contacts | Personal Data Policy | User Agreement | When citing a document, a link to the site indicating the source is required.
Heart diseases
iserdce
Mitral valve insufficiency grades 1, 2, 3: causes, diagnosis and treatment
Each person's heart has four muscular chambers, between which valves are located. Their normal operation ensures directed blood flow. If their function is impaired, a certain amount of blood is retained, which leads to a secondary disruption of the structure of muscle tissue. The mitral valve is located between the atrium on one side and the left ventricle on the other. Its insufficiency is the most common heart defect, however, as a rule, it is accompanied by other changes in the valve apparatus.
Causes
All causes of the development of mitral valve insufficiency are divided into those that appeared during the formation of organs (congenital) and acquired. The latter include:
- rheumatic damage (about 15%);
- scleroderma;
- systemic lupus erythematosus;
- myxomatous degeneration;
- idiopathic chordal rupture;
- Barlow's disease;
- dysfunction of papillary muscles due to ischemia (about 10%);
- valve leaflet calcification;
- infective endocarditis;
- consequences of surgery (valvuloplasty);
- relative secondary failure due to changes in the cavities of the heart (left ventricular aneurysm, dilatation of the left atrium due to ischemia, dilated cardiomyopathy or hypertension);
- mitral valve prolapse.
Among the congenital changes are:
- hereditary pathology of connective tissue (Elens-Danlos and Marfan syndromes);
- disruption of heart formation in the prenatal period;
- splitting of the anterior valve leaflet in the case of an open atrioventricular message.
The causes of the defect may be associated with congenital changes, hereditary pathology, or be a consequence of acquired diseases.
Classification
The leading factor in the pathogenesis of mitral valve insufficiency is reverse blood flow, or regurgitation. Considering the volume of counterflow, there are several degrees of mitral regurgitation:
- Mitral valve insufficiency of the 1st degree is accompanied by a small amount of regurgitation, which is less than 25%. In this case, the countercurrent does not penetrate deeply and remains within the atrioventricular communication. The defect is most often compensated, that is, the patient may not experience any symptoms and feel satisfactory. No changes are detected on the ECG. Only with Doppler ultrasound can you see multidirectional flows and estimate their speed.
- Mitral valve insufficiency of the 2nd degree is already considered a more serious disease, in which secondary changes in the heart muscle can occur. In this case, the volume of regurgitation reaches 50%, and therefore pulmonary hypertension occurs quite often. An increase in the amount of blood in the vessels leads to symptoms (shortness of breath, cough, rapid pulse). Due to the expansion of the boundaries of the heart, changes may appear on the ECG. Pi Doppler can be seen that the reverse flow of blood reaches the middle of the atrium.
- Mitral valve insufficiency of the 3rd degree is considered the most serious problem and, if left untreated, often leads to loss of ability to work and limitation of its capabilities. In this case, the blood stream reaches the posterior wall of the atrium, and the volume of regurgitation can exceed 90%. Essentially, most of the blood entering the ventricle flows back into the atrium and the heart becomes ineffective. In this regard, such a defect is always decompensated. Signs of stagnation appear in both circles of blood circulation. Due to the addition of secondary changes in the myocardium (left ventricular hypertrophy), changes are also detected on the ECG. The borders of the heart are significantly shifted to the left side.
According to the clinical course, mitral valve insufficiency can be acute or chronic. The first type of pathology is usually associated with sudden changes, for example, rupture or ischemia of the papillary muscles during inferior myocardial infarction. The chronic course is characterized by a gradual increase in failure against the background of a sluggish process, for example, with the gradual transformation of the heart with dilated cardiomyopathy or with rheumatic disease.
Symptoms
Symptoms of mitral valve insufficiency in a compensated state may be absent or appear only during intense exercise. Subsequently, during the chronic course of the disease, transformation of the left ventricle gradually occurs, since it bears a large load. This condition leads to expansion of its cavity and thickening of the walls (hypertrophy). First, there is insufficiency of blood flow in the small circle, and then in the large circle. In case of secondary right ventricular failure, it is possible to identify:
- swelling of the lower extremities;
- enlargement of the liver due to venous stagnation;
- accumulation of fluid in body cavities (abdominal, pleural, pericardial);
- arrhythmia, often atrial fibrillation;
- peripheral acrocyanosis and hypoxia.
With the acute development of mitral regurgitation, the heart chambers do not have time to adapt to new hemodynamic conditions, so the symptoms of left ventricular failure come first.
- shortness of breath, which worsens in a horizontal position;
- cardiopalmus;
- cough with pink sputum;
- wet rales;
- pulmonary edema.
All these symptoms can also be observed during decompensation of the chronic form of the disease.
Diagnostics
Already during a routine examination one can suspect a change in the mitral valve:
- the patient’s characteristic complaints allow us to assess the degree of heart failure;
- murmurs are detected on auscultation;
- upon percussion, the boundaries of cardiac dullness shift to the left side.
The main diagnostically significant method for mitral regurgitation is ultrasound of the heart, which can be supplemented with Doppler ultrasound, which allows a more visual assessment of the degree of regurgitation.
With ECHO-CG it is possible to determine the cause of the heart defect, as well as complications of this condition. Based on the measurements obtained, the degree of deficiency can be judged.
It should be noted that isolated mitral valve disease is quite rare and in most cases is caused by rheumatic changes. Much more often, ultrasound of the heart reveals combined insufficiency of the mitral and tricuspid valves. Such changes quickly lead to decompensation of heart failure and require prompt medical intervention.
Auxiliary diagnostic methods are:
- ECG, which changes only with secondary transformation of the heart muscle;
- chest x-ray, which may indicate a general increase in heart size;
- transesophageal ECG helps diagnose atrial rhythm disturbances;
- daily monitoring is performed for paroxysms of arrhythmia;
- phonocardiography allows you to detect noise;
- with ventriculography using special contrast, the degree of regurgitation can be more accurately determined;
- Coronary angiography is performed as preoperative preparation or if the ischemic nature of the defect is suspected.
Treatment
A mild degree of the disease, which is not accompanied by the appearance of symptoms, does not require special treatment.
Moderate mitral valve insufficiency is not an indication for surgery. In this case, treatment is carried out with the help of medications:
- ACE inhibitors prevent secondary transformation of the heart myocardium and reduce symptoms of heart failure;
- beta blockers reduce the frequency of contractions of the left ventricle, thereby increasing the ejection fraction;
- diuretics accelerate the removal of fluid from the body and eliminate symptoms of stagnation;
- Vasodilators reduce the load on the heart by depositing blood and fluid in the peripheral arteries;
- cardiac glycosides stimulate heart contractions and help fight arrhythmia;
- It makes sense to use anticoagulants for persistent atrial fibrillation;
- antibiotics are prescribed for infective endocarditis;
- Hormonal medications can affect the course of rheumatism.
In case of acute development of regurgitation, intra-aortic balloon counterpulsation can be used. During this procedure, a special oval inflating balloon is inserted into the patient's aorta, which opens in opposition to the contractions of the heart. As a result, coronary blood flow increases and the ejection fraction also increases. This measure is temporary and is mainly suitable for ischemia of the papillary muscles, or as preoperative preparation.
For grade 3 mitral valve insufficiency, the only solution is surgical correction of the defect.
Most radical surgery mitral valve replacement is commonly considered. In this case, the chest is opened and the artificial circulation machine is further connected and cardiac activity is temporarily stopped. The installed implant can be made of a metal alloy or be of an organic nature (valve of animal origin). The rehabilitation period after surgery is quite long, but the result is usually good.
In the absence of serious changes in the valve leaflets, treatment can be performed using organ-sparing surgery:
- valve plastic;
- annuloplasty;
- shortening of chords;
- suturing damaged papillary muscles.
Prognosis and prevention
The prognosis for this cardiac defect depends on its cause, the degree of regurgitation, the presence of complications and secondary changes. The average ten-year survival rate is about 60%, which is much higher than for aortic stenosis.
With moderate or mild mitral valve insufficiency, there are no contraindications for pregnancy and childbirth. All patients with this disease should undergo an examination by a cardiologist and an ultrasound scan annually, and more often as new symptoms progress or appear. This will allow you to notice the deterioration of the condition in time and carry out the necessary treatment.
🔻🔻Mitral valve insufficiency - treatment methods, symptoms and signs of pathology
Insufficient functionality of the valve apparatus affects the functioning of the entire body. Mitral valve insufficiency can provoke the development of serious complications and requires treatment.
Symptoms of the pathological process
A feature of the condition is the long-term absence of obvious signs of damage. The heart muscle successfully compensates for the deviation over several years. Defects are often detected during periodic inspections, when characteristic noises are determined. Sound anomalies are formed under the influence of blood flow returning to the left atrium during contraction of the ventricle of the same name.
Against the background of insufficiency, the left-sided ventricle begins to increase in volume - due to pumping more and more of it. Each heart contraction intensifies, the patient feels a palpitation when lying horizontally on the left side.
Next, there is an increase in the left-sided atrium - to be able to accommodate all the blood entering it. The department begins to rapidly contract against the background of atrial fibrillation. The pumping function of the heart is impaired due to a disruption in the rhythm of contractions formed under the influence of mitral insufficiency.
The atria begin to tremble rather than contract, and changes in the circulatory system provoke the formation of blood clots. A pronounced reverse flow of blood provokes the development of insufficient cardiac performance.
Signs of pathology
Symptomatic manifestations of valvular disorder are characterized by:
- a sharp drop in blood pressure levels - up to the appearance of a cardiogenic shock state;
- insufficient functionality of the left ventricle;
- swelling of the lung tissues - a state of suffocation, cough reflex, wheezing and sputum production;
- atrial extrasystoles;
- atrial fibrillation.
Reasons for the formation of pathological deviation
The development of a pathological deviation is observed with changes in the structure or performance of the valve apparatus or heart muscle. The disease is characterized by damage to the valves, muscle tissue or chordae tendineae of the organ. Associated ailments lead to dysfunction of the valve apparatus.
Acute failure is formed under the influence of:
- transformation and destruction of the connective tissue of the mitral valve;
- violation of the integrity of the tendon chords;
- decreased muscle functionality;
- rheumatoid lesions;
- neoplasms in the atria.
The acute form of pathological deviation is not the only option for the development of pathology. The slow and hidden process that causes abnormalities in the heart’s performance can last for decades. Patients with the chronic form do not pay attention to the latent disease.
The chronic version of the disease is provoked by:
- rheumatoid lesions;
- lupus erythematosus;
- infectious and inflammatory processes;
- genetic predisposition;
- inflammatory processes affecting the formation of changes in tissue structures;
- surgical intervention.
Degree of disease development
The disease has several independent classifications that characterize the pathology from all sides. Experts divide mitral regurgitation into three main subtypes:
Mitral regurgitation of the 1st degree - the compensated form is characterized by a reverse outflow of blood of no more than 20% of the total systolic volume. There are no symptomatic manifestations of deviation, the patient does not complain about the general condition.
At conducting an ECG no changes are detected; the examination reveals systolic murmurs and a slight expansion of the borders of the heart to the left side.
Mitral insufficiency of the 2nd degree - subcompensated form - reverse ejection can be recorded in the range from 20 to 50% and lead to congestion in the lung tissues. To push blood out, the body artificially increases blood pressure. Pulmonary hypertension begins to develop.
Symptomatically, the pathology is manifested by shortness of breath, accelerated heartbeat during exercise and in a state of absolute rest, and cough. On ECG decoding changes in the atrium are emphasized. A physical examination reveals non-standard sounds during systole and enlarged borders of the heart muscle: to the left side - no more than 2 cm, to the right and up - up to half a cm.
Mitral insufficiency of the 3rd degree is a decompensated form - the reverse flow of blood flow reaches 90%. Hypertrophy of the left atrium does not allow it to push out the entire volume of blood. The deviation is manifested by tissue swelling, liver enlargement, and increased venous pressure. The heart is maximally dilated, pronounced systolic murmurs are detected.
According to the etiological factor in the formation of the pathological deviation, the types of mitral regurgitation are distinguished:
- congenital - formed during intrauterine development, approximately between 12 and 14 weeks of gestation;
- acquired – damage to the structural elements of an organ occurs during the patient’s life, under the influence of certain specific preconditions.
The following division is carried out according to the reasons for the formation of the disease; among the deviations are:
- organic failure with damage to the valve flaps;
- relative or functional insufficiency - without obvious signs of damage to the structures of the valve leaflets.
The disease can develop at different rates:
- acute form - registered several hours after the formation of a pathological abnormality, provoking changes in the standard performance of the heart;
- chronic - records after a long period of time, after a long pathological process (latent form of damage without obvious symptomatic signs).
Diagnostics
To identify the root causes of insufficient functionality of the valve apparatus, the specialist initially collects medical history data:
- approximate time of first symptomatic manifestations;
- information about close relatives with characteristic lesions of the cardiovascular department - to confirm or exclude the fact of hereditary predisposition;
- previous diagnoses of any etiology;
- Auscultation, percussion, and examination of the condition of the skin are performed.
After the initial diagnosis is made, the patient is sent for laboratory and diagnostic examination:
- clinical urine and blood tests;
- immunological and biochemical tests blood and urine;
- ECG - to determine the rhythm of the heart and identify possible arrhythmic abnormalities;
- echocardiography - a technique that allows you to give a comprehensive description of the condition of the organ and nearby vessels;
After receiving all the necessary results, the cardiologist prescribes the necessary individual therapy.
Treatment methods for mitral valve insufficiency
For minor or moderate forms of the pathological process, specialized therapy is not prescribed. The patient is advised to reconsider his usual lifestyle and periodically visit a cardiologist to prevent further progression of the disorder.
In all other cases, treatment is aimed at suppressing the symptomatic manifestations of the underlying disease, which served as a prerequisite for the development of mitral regurgitation. Experts prescribe one of the treatment options - conservative or surgical.
Medication
Required medications are prescribed according to an individual scheme, depending on the general condition of the patient, his age, and the severity of the disease. Commonly prescribed medications include:
- anticoagulants - prescribed to reduce blood density;
- antiplatelet agents – necessary to prevent the formation of blood clots;
- beta blockers - stabilize blood pressure, improve the functioning of the heart muscle;
- diuretics – prevent swelling of tissues, promote the removal of excess fluid from the body;
- ACE inhibitors - used to reduce the level of vascular resistance.
The duration of treatment depends on the level of damage by the pathological process.
Surgical procedures
Surgical manipulations are necessary in case of severe damage to the mitral valve and severe insufficiency of its functionality.
Plastic surgeries are prescribed at the second and third stages of the disease. Three manipulation options are used:
- valves - a support ring is sewn at their bases;
- decrease in chord length;
- excision of the elongated part of the posterior valve.
Prosthetics – replacement of a damaged valve with artificial or natural material. This type of intervention is most often prescribed to children and women who plan to bear a baby in the future.
Surgical techniques are prohibited for use in cases of severe damage, in case of insufficient performance of the heart muscle, which is not amenable to drug influence.
Non-drug
Widely practiced traditional methods treatments are completely unsuitable for the treatment of cardiovascular pathologies. Herbs and decoctions are not capable of seriously affecting an already damaged valve apparatus, and refusal of official medications will lead to the development of complications and further death.
- stop drinking alcoholic and low-alcohol drinks;
- cure nicotine addiction;
- change your daily schedule - get up and go to bed at the same hours, maintain a nightly sleep time of at least 8 hours;
- go to the recommended dietary table;
- monitor your body weight - any extra pounds have a negative effect on the heart, creating additional stress for it.
Treatment tables
A balanced diet that ensures sufficient intake of vitamins and minerals into the patient’s body is one of the important points in the prescribed treatment. The therapeutic table is based on the following principles:
- moderation in portion sizes;
- fractional meals - about six meals a day, with a volume of 200–250 ml each;
- elimination of foods high in animal fats, cholesterol and table salt.
Patients are prohibited from having dinner later than three hours before going to bed. To prepare dishes, methods of cooking, steaming, and stewing are used.
Certain types of products are strictly prohibited:
- varieties of meat with a high fat content - pork, lamb, beef;
- animal by-products;
- dairy products – sour cream, hard cheeses, cream;
- chicken eggs;
- white breads and pastries;
- sweet tea or coffee;
- chocolate and confectionery products.
Salty or spicy foods provoke an increase in appetite and an increase in portions, which is strictly prohibited in case of cardiovascular diseases. Nutritionists advise spending a certain period on a salt-free diet to reduce tissue swelling.
Prognosis for recovery
The chances of returning to normal life depend on the root cause of the development of the pathological process.
The prognosis will be unfavorable if the underlying diseases are not treatable and continue to progress slowly. The following ailments can lead to hemodynamic disturbances and other damage to the heart muscle and internal organs:
- rheumatoid pathologies;
- lupus;
- ischemic damage to the heart muscle, etc.
If the valve device is damaged by endocarditis or degenerative changes in the valve apparatus, the prognosis is conditionally favorable. Cure is guaranteed with timely surgical intervention - valve replacement or valve repair. The service life of a valve prosthesis is calculated from 8 to 20 years, depending on the material of manufacture.
In the presence of the first degree of severity, which is not accompanied by problems with the circulatory system, the prognosis is considered favorable. When correctly assigned conservative treatment and constant monitoring tactics, mitral insufficiency may be “mothballed” for many years.
Prevention of mitral valve insufficiency
To prevent the development of pathological deviations, experts recommend adhering to a number of rules:
- carry out measures to harden the body;
- attend consultations with a cardiologist and rheumatologist in a timely manner;
- adhere to recommended nutritional principles;
- treat the underlying disease.
With an existing process, follow preventive actions to prevent its progression. Patients must carefully follow all specialist prescriptions, both during medicinal and surgical treatment.
MVC or mitral valve insufficiency is a serious illness, ignoring the primary signs of which can lead to a disability group. Bicuspid valve prolapse and other lesions increase the risk of death. Timely treatment and compliance with its standards will give the patient a chance to prolong his life.
The inability of the mitral valve to prevent the reverse flow of blood received its ICD code - I34.0.
Interferon status (IFN status) is a set of a number of indicators (parameters) characterizing the state of the main system of innate (nonspecific) immunity - the IFN system, its reactivity and functional activity, which provides the first line of defense of the body from various infectious (and non-infectious) agents recognized cells as an alarm signal.
Infection with various pathogens causes a protective response in cells with the synthesis of universal protective proteins - IFNs, which prevent and/or interrupt the spread of the infectious process, stimulate innate and adoptive immune responses and maintain the homeostasis of the body as a whole. The universal phenomenon of IFN formation is inherent in the cells of almost all vertebrates from fish to humans; viruses are natural inducers of IFN.
Recognition of viral and microbial structures, known as pathogen-associated molecular patterns (PAMPs), is carried out by the so-called pattern recognition receptors (PRR), which include the most studied Toll-like receptors (TLRs), which play a key role in the activation of the IFN system in viral or bacterial infections and in the associated induction of other parts of the innate immune response.
TLRs are sensitive to a wide range of viruses, bacteria, fungi and protozoa. The interaction of various pathogens with the corresponding TLRs activates signaling pathways for the expression of IFN genes, which mediate the induction of the innate immune response of the IFN system, promoting the production of other Th1 proinflammatory cytokines (TNF-α, IFN-γ), the development of the cellular immune response and adaptive immunity.
The variety of physiological functions of IFN discovered to date and the universal ability of different cells to produce different types of IFN indicate the existence in each cell of an IFN system, which is aimed at protecting against foreign genetic information and ensuring nucleic acid homeostasis of the body as a whole.
Implemented at the molecular and cellular levels, the IFN system forms a protective barrier against infectious agents much earlier than specific protective reactions of the immune system. The course and outcome of the disease depend on the speed and efficiency of switching on the IFN system in various forms of pathology. A timely, adequate response from the IFN system can ensure the elimination of pathogens from the body without the participation of a slower-responding adaptive immune system associated with the need to accumulate a clone of antigen-specific immune cells and antibodies. Delayed or reduced production of endogenous IFNs can lead to progression or chronicity of the disease, including death.
A reflection of the reactivity and functional activity of the IFN system is the IFN status, which includes the determination of 4 main indicators:
1. the level of production of IFN-α by blood leukocytes upon its induction in vitro by the standard IFN-α inducer - Newcastle disease virus (NDV). A load test that characterizes the IFN-α-producing ability of the patient’s blood leukocytes, in which the infection of his blood leukocytes with NDV is simulated in vitro and the amount of the protective protein produced by them, IFN-α, is determined;
2. the level of production of IFN-γ by blood leukocytes upon its induction in vitro by the standard IFN-γ inducer – phytohemagglutinin (PHA). A load test characterizing the IFN-γ producing ability of the patient's blood leukocytes, in which the interaction of blood leukocytes with the mitogen - PHA - is simulated in vitro and the amount of the protective protein produced by them - IFN-γ - is determined;
3. the level of spontaneous IFN production by blood leukocytes in vitro in the absence of any additional induction;
4. quantitative content of IFN circulating in the blood serum.
The combination of these indicators characterizes the state of the IFN system and the patient’s immunoreactivity in situ. Violations in various parts of the IFN system are determined by:
- acute and chronic viral and other intracellular infections;
- allergic, autoimmune, oncological diseases;
- recurrent acute respiratory viral infections and tonsillitis in frequently ill children;
- secondary immunodeficiencies associated with other forms of pathology.
All of the above diseases are indications for studying IFN status.
The study of IFN status indicators allows us to identify the following disorders in the IFN system of the studied patients:
- an increase in serum IFN titers associated with a decrease in the production of IFN-α and/or IFN-γ by blood leukocytes, indicating the acute stage of the disease;
- a decrease in the α- and γ-IFN producing ability of blood leukocytes in combination with the absence of serum IFN circulating in the blood, indicating a defective IFN system;
- a decrease in the α- and γ-IFN-producing ability of blood leukocytes in combination with the presence of spontaneous IFN production and the absence of IFN circulating in the blood, indicating a persistent viral or other intracellular infection.
Depending on the degree of reduction of the 2 most significant indicators IFN status - the level of production of IFN-α and IFN-γ by blood leukocytes in vitro relative to the physiological norm; 4 degrees of insufficiency of the IFN system are distinguished according to the α- and/or γ-links of the IFN system, respectively:
- 1st degree – 2–4-fold decrease in the production of IFN-α and IFN-γ compared to the lower limit of the physiological norm;
- 2nd degree – 4–8 fold reduction;
- 3rd degree – 8–16 fold reduction;
- 4th degree – 16 or more fold reduction.
In case of insufficiency of the IFN system accompanying various forms of pathology in children and adults, it is necessary to carry out corrective IFN-stimulating therapy aimed at correcting the reduced production of α - and γ -IFN, modulating the functional activity of the IFN system and innate immunity, associated adaptive immunity and rehabilitation of the patient the body as a whole.
To select an adequate immunotropic drug and subsequent effective immunocorrective therapy, additional studies are required to determine the individual sensitivity of the patient's blood leukocytes to IFN drugs, IFN inducers or immunomodulators. Individual sensitivity studies are usually carried out in parallel with an in situ study of IFN status.
Individual sensitivity to drugs is studied based on the effectiveness of the corrective effect of the drug (correction coefficient) on the initially reduced production of IFN-γ by the patient’s blood leukocytes - the key cytokine that determines the direction, intensity and effectiveness of the body’s interferon and immune response to infectious agents (RF patent No. 2423705, 2009 .).
Depending on the values of the correction factor, there are 5 options for individual sensitivity to immunoactive drugs:
- 2 – weak; an increase in the production of IFN-γ by the patient’s blood leukocytes in the presence of the drug relative to the original by 2 times;
- 4 – pronounced; an increase in the production of IFN-γ by the patient’s blood leukocytes in the presence of the drug relative to the original by 4 times;
- more than 4 – very pronounced; an increase in the production of IFN-γ by the patient’s blood leukocytes in the presence of the drug relative to the original by more than 4 times;
- 1 – lack of sensitivity; an increase in the production of IFN-γ by the patient’s blood leukocytes in the presence of the drug relative to the initial one is not tested;
- less than 1 – immunotoxicity; suppression of IFN-γ production by the patient’s blood leukocytes in the presence of the drug relative to the original.
The study of IFN status with determination of the individual sensitivity of the patient’s blood leukocytes to immunoactive drugs allows the attending physician to obtain advanced information about the effectiveness of subsequent immunocorrective therapy and make the correct scientifically based choice of a drug or combination of drugs that is adequate for this particular patient.
The use of IFN drugs, IFN inducers or immunomodulators combines well with antibiotics, antivirals and other drugs of basic therapy, increases the effectiveness and reduces the duration of treatment for the patient.