Subclinical hypothyroidism is a form of thyroid dysfunction without symptoms. The disease is detected by determining blood hormones. Older women are most susceptible to subclinical hypothyroidism.
The main sign indicating the presence of the disease is increased amount thyroid-stimulating hormone of the pituitary gland in the blood. The thyroid-stimulating hormone of the pituitary gland is responsible for regulating the secretion of thyroid hormones, therefore, when even a slight decrease in thyroid function occurs, an increase in the thyroid-stimulating hormone of the pituitary gland is observed, while the amount of thyroid hormones in the blood may be normal or slightly reduced.
Signs of hypothyroidism
Unfortunately, diagnosing hypothyroidism is the number one problem. Many patients suffer from hypothyroidism. however, often clinical picture the disease is carefully disguised, while the patient may exhibit the following symptoms?
Gastroenterology:
- Constipation
- Manifestations of gallstone disease
- Biliary dyskinesia
Rheumatology:
- Syneviitis
- Polyarthritis
- Manifestations of progressive osteoarthritis
Gynecology:
- Infertility
- Uterine bleeding
Cardiology:
- Diastolic hypertension
- Cardiomegaly
- Bradycardia
With subclinical hypothyroidism, there are no signs of dysfunction of the thyroid gland, but deviations from the norm in metabolism may be observed. For this reason, other functions in the body may suffer. Patients often experience a decrease in mood, depression, anxiety, memory impairment, decreased concentration, weakness, and fatigue.
Fat metabolism in subclinical hypothyroidism does not go unnoticed. This manifests itself in an increase in body weight, the development of atherosclerosis, coronary heart disease, and a high risk of heart attack. Replacement therapy for initial stage diseases in some cases helps restore metabolic processes.
Thyroid hormones affect the circulatory system, namely the circulatory organs. The influence of hormones can change the number of heart contractions, myocardial contractility, blood pressure, blood flow speed, and blood vessel resistance. With subclinical hypothyroidism, hypertrophy of the heart muscle in the area of the left ventricle may be observed, which indicates overstrain of the heart.
It is very important to identify subclinical hypothyroidism during pregnancy, since early detection of the disease makes it possible to avoid disturbances in the fetus’s body, thanks to timely treatment.
Symptoms of subclinical hypothyroidism
- Memory impairment
- Decreased concentration
- Decrease in intelligence
- Susceptibility to depression
- Increased level of endothelial dysfunction
- Rhythm disorders
- Violations menstrual cycle
- Vaginal bleeding
- Infertility
- Premature birth
- Increased intraocular pressure
- Hypochromic anemia
- Myalgia
Treatment of subclinical hypothyroidism
Replacement therapy may be prescribed. Although many doctors argue that subclinical hypothyroidism does not require treatment. But the disease is fraught negative consequences Therefore, after comparing the symptoms, the doctor decides on the need for treatment.
L-thyroxine (levothyroxine) is often used in the treatment of subclinical hypothyroidism. L-thyroxine is especially important for expectant mothers. In the absence of a history of thyroid surgery, doctors often postpone treatment in order to monitor the patient’s condition and require repeated tests in a couple of months. If there are no changes, treatment will be prescribed.
When taking l-thyroxine, most patients notice improvements, but taking the drug can result in a lot of pain. side effects, among them there is an increase in body weight, anxiety, insomnia, arrhythmia, tachycardia.
It is very important to compare possible complications without treatment of subclinical hypothyroidism with the effectiveness of the drug, and one should not discount its side effects. The decision on the need for treatment is made by the doctor if the first two points are equivalent. However, before starting treatment, it is necessary to exclude transient hypothyroidism.
The most interesting news
Thyroid diseases - Diet
Read more about this disease in the section. THYROID
Thyroid diseases in women are 8-20 times more common than in men. And a disease such as thyroiditis occurs 15-25 times more often in women than in men. In addition, the volume and weight of the gland in women can fluctuate depending on the menstrual cycle and pregnancy. In the absence of thyroid disease in men, her weight is constant.
Diseases of this type in women and men most often occur at the age of 30-50 years. Disorders of this organ also occur in children, and they can also be congenital. Enlargement of the gland in children due to iodine deficiency in some areas reaches 60-80%. Thyroid dysfunction affects 3% of the population.
The most common thyroid diseases are: hypothyroidism, hyperthyroidism, autoimmune thyroiditis, nodular goiter, cyst, cancer.
Hypothyroidism of the thyroid gland - causes, symptoms
Hypothyroidism- decreased activity of the thyroid gland. One of the reasons is iodine deficiency, which reduces hormone synthesis. Other causes of this disease are developmental abnormalities, inflammation of the gland, congenital defects in the synthesis of hormones
Symptoms of hypothyroidism:
Fatigue and loss of strength, chilliness, weakness, drowsiness, forgetfulness, decreased memory, hearing, dry and pale skin, swelling, constipation, excess weight, the tongue thickens, impressions from the teeth are noticeable at the edges, and hair begins to fall out.
With this disease, the menstrual cycle may be disrupted in women; in men, potency is impaired and libido decreases.
The disease develops slowly, over the years, the symptoms of hypothyroidism are not noticeable for a long time
Hyperthyroidism - causes, symptoms
Hyperthyroidism (thyrotoxicosis)– increased activity of the thyroid gland. With this disease, the iron produces an excess amount of hormones, which leads to “poisoning” of the body with these hormones - thyrotoxicosis. Metabolism increases. Increases thyroid. The cause of hyperthyroidism cannot be excess iodine, since the excess is excreted by the kidneys. The causes are mental or physical stress, disease of other organs, hereditary predisposition, pituitary tumor
Symptoms of hyperthyroidism of the thyroid gland:
Weight loss, feeling hot, sweating, trembling hands, irritability, anxiety, rapid heartbeat, feeling of “sand” in the eyes, pressure behind the eyes.
Carbohydrate metabolism is disrupted, which can lead to diabetes mellitus 2nd type
In women, the menstrual cycle may be disrupted, in men, potency is disrupted.
The disease develops very quickly.
Autoimmune thyroiditis, causes, symptoms
Thyroiditis– inflammation of the thyroid gland.
Autoimmune thyroiditis caused by a buildup of white blood cells (leukocytes) and fluid inside the gland. In autoimmune thyroiditis, antibodies produced by the immune system mistake the cells of one's own thyroid gland for foreign ones and damage them. There is a gradual destruction of the thyroid gland, which leads to hypothyroidism. Also, against the background of autoimmune thyroiditis, a temporary increase in hormone production is possible - hyperthyroidism
Cause of this disease- partial genetic defect of the immune system. This defect may be hereditary, or may be caused by poor ecology, pesticides, an excess of iodine in the body (long-term excess of iodine stimulates the production of antibodies to thyroid cells), radiation, infections
Symptoms— autoimmune thyroiditis:
During the first years of the disease there are no symptoms, then symptoms of hyperthyroidism may temporarily appear, and then symptoms of hypothyroidism. The main symptoms of this disease are associated with its inflammation and enlargement: difficulty swallowing, difficulty breathing, pain in the thyroid gland
Goiter - causes, symptoms
Goiter is a disease characterized by a pathological increase in the volume of the thyroid gland. Goiter occurs as a result of increased cell proliferation in order to increase the production of the missing thyroxine due to this increase. One of the reasons is iodine deficiency. Goiter can develop in both hypothyroidism and hyperthyroidism
Thyroid nodules and nodular goiter are formations that differ from the gland tissue in structure and structure. All nodular forms of thyroid diseases are divided into two groups: 1) nodular colloid goiter, which never degenerates into cancer; 2) tumors. Tumors, in turn, can be benign, in which case they are called adenomas, and malignant, in which case they are called cancer.
Thyroid cancer
easy to diagnose, often detected on early stages using puncture biopsy of nodes. Symptoms of thyroid cancer (sore throat and neck, pain when swallowing and breathing) are sometimes attributed to infectious diseases, so in some cases diagnosis is difficult. The chance of recovery from thyroid cancer is more than 95% if the disease is diagnosed at an early stage.
Diet for thyroid diseases
Diet for the treatment of the thyroid gland vegetarian preferably. It is necessary to include more greens, root vegetables, fruits, nuts, and vegetable proteins in your diet. They contain the necessary organic iodine.
The diet for a thyroid disease such as hypothyroidism should contain fish, seafood, and seaweed. These products have the highest iodine content - 800 - 1000 mcg/kg ( daily requirement in iodine - 100-200 mcg).
Here's another foods containing iodine in large quantities: beans, soybeans, green peas, carrots, tomatoes, radishes, lettuce, beets, potatoes, garlic, apple seeds, grapes, persimmons, millet, buckwheat. (40-90 mcg/kg). The iodine content in products of plant origin also depends on the soil on which these products are grown. In vegetables grown on iodine-rich and iodine-poor soils, the iodine content can differ many times.
When treating the thyroid gland, the diet should include foods rich in the following microelements: cobalt, copper, manganese, selenium. They contain a lot of chokeberries, rose hips, gooseberries, blueberries, strawberries, raspberries, pumpkin, eggplant, garlic, black radish, turnips, beets, and cabbage.
According to some theories, it is believed that the main cause of thyroid problems is pollution in the body. With hyperfunction of the gland, thyrotoxicosis, the lymph is so contaminated that it cannot cope with the drainage of this organ. Polluted blood constantly irritates the gland with its toxins; therefore, it is no longer able to be controlled by the pituitary gland, and malfunctions occur in its functioning. The presence of toxins in the blood that are harmful to the thyroid gland is associated with pollution, poor liver and intestinal function. In addition, it is believed that one of the causes of hypothyroidism is a violation of the absorption of iodine and other nutrients in the intestines, and the cause of hyperthyroidism can be untimely evacuation of iodine from the body. In connection with this theory, the diet should be such as to cleanse the blood, liver and intestines and improve their functioning. Therefore, it is useful to drink teas from bitter herbs (wormwood, angelica root, yarrow, St. John's wort), cleansing products (radish, garlic, horseradish, celery, parsnips, nuts)
Diet for thyroid diseases should not include the following products:
1. Fatty meat, sausages.
2. Margarine; artificial fats.
3. Sugar, confectionery.
4. White bread, pastries, baked goods
5. Fried, smoked, canned foods
6. Spicy seasonings: mayonnaise, vinegar, adjika, pepper
7. Chemical substances: dyes, flavors, flavor enhancers, stabilizers, preservatives
8. Avoid smoking and drinking alcohol and coffee.
The basis of nutrition There should be porridge, boiled and fresh vegetables, legumes, fruits, vegetable oil. In small quantities diet may contain: honey, butter, nuts, eggs
Diet for hypothyroidism
Do not use folk remedies without consulting a doctor! Remember that all methods may have individual contraindications.
More articles about this disease:
Hypothyroidism
Hypothyroidism is a condition that is caused by an inadequate decrease in the concentration of free thyroid hormones in the blood serum.
In our clinic, we successfully treat this disease using hirudotherapy. in a few sessions of complex therapy you will feel the disease receding. Read the article on this disease.
Because thyroid hormone receptors are present in virtually all tissues, the signs and symptoms of hypothyroidism are many and varied. The severity of clinical manifestations depends on the degree of decrease in T3 and T4 concentrations. Severe hypothyroidism is designated by the term “myxedema,” in which there is an accumulation of hydrophilic mucopolysaccharides in the basal layers of the skin and other tissues.
There are primary, secondary and tertiary hypothyroidism. Primary hypothyroidism is caused by direct damage to the thyroid gland, which results in the development of insufficiency of its function,
Secondary hypothyroidism is a consequence of hypofunction of the pituitary gland and insufficient production of thyroid-stimulating hormone (TSH), decreased TSH stimulation of thyroid function and insufficient synthesis of T4, T3.
Tertiary hypothyroidism develops as a result of pathology of the hypothalamus, a decrease in the synthesis of thyrotropin-releasing hormone (TRH) and insufficient stimulation of the pituitary thyrotrophs, a decrease in the synthesis of TSH and stimulation of TSH of the thyroid gland.
Hypothyroidism is characterized by a wide range of disorders and damage to various body systems. Their presence and severity depend on the severity of hypothyroidism. Damage of cardio-vascular system observed in 70-80% of patients. The nature and extent of cardiac changes depend on the age of the patient, the etiology of hypothyroidism, and concomitant diseases.
The most pronounced changes in the cardiovascular system occur with severe primary hypothyroidism and are referred to as “myxedematous heart”, the first clinical description of which was given by H. Zondek in 1918, highlighting its main symptoms - cardiomegaly and bradycardia.
It has been established that T3 acts on specific myocyte genes responsible for the function of cardiomyocytes, affects myosin, Ca-activated ATPase of the sarcoplasmic reticulum, phospholamban, adrenergic receptors, adenyl cyclase and protein kinase. Both T3 stimulation and T3 deficiency affect myocardial function, including contractility, mass, and number of contractions.
With hypothyroidism, protein synthesis decreases, the concentration of sodium and water ions increases, the content of potassium ions decreases, hypo- or hyperchromic anemia develops due to a decrease in oxidative processes and protein synthesis in the bone marrow, and capillary permeability increases. An increase in capillary permeability plays a major role in the development of edema of various tissues and organs and, in that number, myocardium and fluid accumulation in the pericardium. With successful replacement therapy, capillary permeability is normalized and symptoms associated with edema are regressed.
Hypothyroidism is accompanied by hypercholesterolemia, resistant and refractory to treatment with diet, statins, and other antihyperlipoprosemic drugs, and the degree of its severity also depends on the severity of the disease. Atherogenic lipid fractions accumulate in the blood, and the level of HDL decreases, which contributes to the rapid and progressive development of atherosclerosis with multiple localizations. Lipid metabolism disorders are found not only in overt hypothyroidism, but also in its subclinical forms.
Cardiac changes are caused by the development of myocardial dystrophy due to a pronounced disturbance of metabolic processes, which progresses as the edema of the stroma and parenchyma in the myocardium increases and is accompanied by a decrease in oxidative phosphorylation, a decrease in oxygen uptake by the myocardium, a slowdown in protein synthesis, and electrolyte disturbances, which leads to a decrease in the contractile function of the myocardium and an increase in heart size, development of heart failure. The size of the heart increases both due to interstitial edema and nonspecific inflammation of myofibrils, dilatation of its cavities, and due to effusion in the pericardium. With timely and adequate treatment of hypothyroidism with thyroid hormones, myocardial dystrophy undergoes reverse development with the complete disappearance of existing signs of heart damage; otherwise, cardiosclerosis develops.
Clinical manifestations cardiovascular disorders in hypothyroidism, they are characterized by complaints of pain in the heart region of a polymorphic nature, shortness of breath during physical activity, arising against the background of various and nonspecific complaints (muscle weakness, decreased mental and motor activity, edema of various localizations). With hypothyroidism, there are two types of pain in the heart, clinically difficult to distinguish: truly coronarogenic (especially in elderly patients), which can become more frequent and intensify when thyroid therapy is prescribed, and metabolic, which disappear during treatment.
During the examination, bradycardia (up to 40 beats/min) or other heart rhythm disturbances are detected.
Sinus bradycardia is recorded in 50-60% of patients with hypothyroidism and is caused, according to researchers, by a decrease in the concentration of blood catecholamines and the sensitivity of adrenergic receptors to them. In 20-25% of patients with hypothyroidism, sinus tachycardia is detected, the pathogenesis of which remains controversial. Most authors explain the presence of sinus tachycardia by a complex of disorders that develop with hypothyroidism - hypothyroid myocardial diatrophy, accompanied by mucous edema of the myocardium, deficiency of macroergs and potassium ions in cardiomyocytes, increased lipid peroxidation and membrane damage, and, consequently, electrical instability of the myocardium, its pseudohypertrophy , accumulation of creatine phosphate, atherogenesis, disturbance of the rheological properties of blood and microcirculation (Tereshchenko I.V.). As a result, in patients with hypothyroidism, especially in old age, in addition to tachycardia, paroxysmal tachycardia, paroxysms of atrial fibrillation and flutter, and sick sinus syndrome may develop. It is noted that these rhythm disturbances are refractory to cordarone and β-blockers and their disappearance when thyroid hormone preparations are prescribed.
Among other rhythm disturbances, it should be noted extrasystole (ES), detected among 24% of patients (atrial - in 15%, ventricular - in 9%). ES occurs more often when hypothyroidism is combined with cardiac pathology (hypertension, coronary artery disease, heart failure, cardiomyopathy). Rhythm disturbances can occur during treatment of hypothyroidism with thyroid drugs, which may be due to increased sympathetic influences on the myocardium under the influence of TG during this period.
During percussion and auscultation of the heart, an increase in cardiac dullness, a weakening of the apical impulse and heart sounds are noted; an accent of the 2nd tone over the aorta can be heard, as a manifestation of atherosclerosis and systolic murmur at the apex of the heart, caused by dilatation of the left ventricle. In the presence of pericardial effusion, heart sounds become muffled and even difficult to hear when there is a significant accumulation of effusion.
X-ray reveals an increase in heart size varying intensity, weakening of its pulsation, expansion of the shadow of blood vessels, signs of fluid accumulation in the pericardium and in the pleural cavities (the heart takes the shape of a “decanter”, its pulsation is sharply weakened). Since transudate accumulates slowly and its amount is not large, cardiac tamponade is rare.
The fluid in the pericardium contains large amounts of protein, unlike the fluid in heart failure. The accumulation of transudate is caused by increased capillary permeability and hypernatremia. It has been established that the transudate is transparent, brown or yellow, contains albumin, cholesterol and mucoid substance, erythrocytes, lymphocytes, monocytes, polynuclear and endothelial cells. The clinical manifestations of hydropericarditis are mild, despite the accumulation of a large amount of fluid, which, according to clinicians, may be due to its slow accumulation. A protodiastolic gallop rhythm (III sound) and, rarely, a IV sound can be heard, as confirmation of a decrease in myocardial contractile function, in the absence of other signs. A small effusion in the pericardium may not change the x-ray picture and its detection can be carried out using a more reliable research method - echocardiography
During an ECG study, various changes are observed. According to researchers, the most common and early sign is a decrease in amplitude, smoothness or inversion of T waves, mainly in leads V3.6, but can also occur in standard leads. These ECG changes occur in 65-80%, regardless of the age of patients ( even in childhood), are not associated with risk factors clinical manifestations atherosclerosis of the coronary arteries - hypercholesterolemia, angina pectoris and arterial hypertension. The second most common ECG sign is a low-voltage waveform, characterized by a decrease in the amplitude of the QRS complex. Its greatest decrease is recorded in the presence of effusion in the pericardial cavity. Depression of the ST segment and a decrease in the amplitude of the P wave may be observed. Intraventricular blockade and prolongation of atrioventricular conduction are diagnosed. Changes in the T wave and ST segment decrease or disappear along with clinical manifestations when adequate replacement therapy is prescribed and remain in elderly patients suffering from coronary disease hearts.
An echocardiographic study in patients with hypothyroidism reveals asymmetric hypertrophy of the interventricular septum, a decrease in the rate of early diastolic closure of the anterior leaflet mitral valve, an increase in end-diastolic pressure, which disappear after pathogenetic treatment.
Decreased myocardial contractile function in hypothyroidism
causes hemodynamic disturbances, which are characterized by a decrease in stroke and cardiac output, a decrease in cardiac index with a reduced volume of circulating blood, as well as an increase in total peripheral resistance in the systemic circulation and diastolic pressure, a decrease in pulse pressure and blood flow velocity in various organs. A long course of uncompensated hypothyroidism can contribute to the development of heart failure, which can be relieved by the prescription of only thyroid hormones with a moderate degree of its severity. Severe stage (IIb and III) of heart failure requires additional prescription of cardiac glycosides, diuretics and indicates the presence of concomitant cardiac pathologies: ischemic heart disease, cardiosclerosis, cardiomyopathy, etc.
Researchers, even in latent, subclinical forms of the disease, identify endothelial dysfunction based on a decrease in endothelial vasodilation (EV), as a marker of early atherosclerosis. When studying the relationship between EV levels and the level of thyroid-stimulating hormone (from O.4 µU/ml), the greatest decrease in vasodilation was observed in patients with TSH levels more than 10 µU/ml (Gavrilyuk V.N. Lekakise J,). Research conducted by Japanese authors to study the thickness of the inner and middle shells of the general carotid artery in 35 patients with hypothyroidism, its thickening was established compared to individuals in the control group (0.635 mm and 0.559 mm, respectively).
Cardiac disorders, which are characterized by the development of myocardial dystrophy in patients with hypothyroidism, should be differentiated, first of all, with ischemic heart disease and atherosclerotic cardiosclerosis, especially in elderly patients and the elderly, since their ECG data may be identical. For this purpose, it is necessary to determine the function of the thyroid gland by studying the levels of hormones in the blood - T3, T4 (preferably their free forms), TSH. Hypothyroidism is confirmed by low level thyroid hormones and their ratio. Differential diagnosis These pathologies based on clinical parameters are presented in Table. 3.
An additional diagnostic test in patients with hypothyroidism with nonspecific ECG changes (which manifests itself in disruption of repolarization processes - smoothed or negative T waves in most leads) is a potassium test, even with normal values of potassium in the blood plasma.
Instrumental diagnostics should be aimed at assessing the functional state of the heart, identifying early signs of heart failure, and excluding the presence of exudate in the pericardial cavities and pleural cavities. For this purpose it is necessary conducting an ECG, daily monitoring of blood pressure and ECG, assessment of heart rate variability, X-ray examination and echocardiography.
The use of 24-hour ECG monitoring and recording of a cardiointervalogram is of particular importance in monitoring treatment with I thyroxine and in assessing its effect on the condition of the heart, since such patients often complain of palpitations and the presence of vegetative manifestations (attacks of sweating, anxiety, trembling, etc.). These methods make it possible to verify episodes of tachycardia, identify other heart rhythm disturbances throughout the day, and check their relationship with the activation of the sympathetic division of the ANS.
Treatment of cardiac manifestations of hypothyroidism is based on the use of thyroid hormone replacement therapy (?-thyroxine, thyroidin, thyroid therapy). The most radical is the use of β-thyroxine at a dose of 1.6 mcg/kg body weight per day. For ischemic heart disease and hypertension, the initial dose should not exceed 15-25 mg with a gradual increase to the optimal dose.
Due to the long half-life of the hormone, levothyroxine is usually taken once a day. On average, 80% of the dose taken is absorbed and absorption worsens with age. The dose of the drug must be selected gradually, individually, starting with the minimum (0.05 mcg/day) dose. For ischemic heart disease and arterial hypertension, the initial dose should not exceed 15-25 mcg/day. The interval between periods of increasing the drug is 2-3 weeks. Today, it is necessary to prescribe L-thyroxine in a dosage that will maintain the TSH level not only normal (0.4-4 mIU/l), but even within a lower range - 0.5-1.5 mIU/ l (Fadeev V.V.), based on the fact that in most people the TSH level is normally 0.5-1.5 mIU/l.
In patients with subclinical hypothyroidism with a TSH level greater than 10 honey/l, the administration of thyroxine preparations is also indicated (Kamenev 3.). In cases of TSH values less than the specified value, the data multicenter studies do not provide a clear conclusion about the usefulness of this treatment.
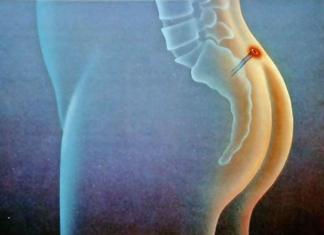
Numerous clinical and pathological studies have proven the increased sensitivity of the myocardium to thyroid hormones. When exposed to thyroid hormones (TH), as a result of increased metabolic processes, relative coronary insufficiency can develop in the absence of atherosclerosis of the coronary arteries (Fig. 4). If you have coronary artery disease in old age, there is a risk of increased frequency of angina attacks and its transition to an unstable form. Treatment with inadequate doses of TG can lead to complications such as myocardial infarction and heart failure. Therefore, it is especially important when prescribing this type of treatment to select adequate doses of thyroid hormones with lengthening the period of adaptation of the body (increase the dose of the drug every 7-12 days) to these hormones and carry out electrocardiographic monitoring every 3-5 days to exclude signs of deterioration of coronary circulation.
The body's need for thyroid hormones decreases in the summer, which must be taken into account when treating patients. Men have a higher average need for thyroxine than women. To assess the adequacy of the replacement therapy, periodic monitoring of the level of TSH in the blood is necessary, an increase in which indicates insufficient treatment, and an increase in T3 indicates excess. In diagnosing an overdose of thyroid drugs, the clinical picture is of primary importance, and this is, first of all, tachycardia and determination of the level of thyroid hormones. At the same time, the content of T4 in the blood serum, according to E. Braunwald and co-author, should be set at a level slightly exceeding upper limit normal fluctuations. Serum T3 concentration is a more reliable indicator of metabolic status in patients receiving levothyroxine than T4 concentration.
When prescribing thyroxine, it is important to teach patients self-control - it is necessary to take into account changes in pulse, blood pressure, body weight, monitor your well-being and tolerability of the drug, which will help avoid complications of hypothyroidism and side effect replacement therapy.
In patients with coronary heart disease, the administration of thyroid hormones must be combined with antianginal drugs: nitrosorbide, nitrong, cordiket, and other β-adrenergic blockers. -Adrenergic blockers reduce the increased TG demand of the myocardium for oxygen and thereby prevent the occurrence of angina attacks (Starkova N.T. Levine H.D. Leading). The use of β-blockers is recommended to be prescribed along with TG to patients with hypothyroidism in combination with arterial hypertension and tachycardia, if rhythm disturbances occur. However, it should be taken into account that β-blockers, along with rauwolfia and clonidine, as well as estrogens, reduce the function of the thyroid gland, aggravating thyroid insufficiency (Tereshchenko I.V.). When rhythm disturbances occur while taking TG, various classes of antiarrhythmic drugs are used.
It should be noted that the use of thyroid therapy alone leads to a decrease or normalization of blood pressure in patients previously unsuccessfully treated with antihypertensive drugs. The combined use of thyroid drugs together with antihypertensive drugs can significantly reduce the doses of the latter (Starkova N.T.).
Correction of thyroid insufficiency relieves patients from hypercholesterolemia without the use of any other drugs, however, it may be necessary to prescribe statins or fibrates.
Treatment of heart failure should be combined with the administration of glycosides and diuretics. Their use is recommended to be combined with the prescription of potassium supplements, given the presence of hypokalemia in patients with hypothyroidism. In the presence of pericardial effusion, puncture is rarely used, since the effusion accumulates in a volume of less than 500 ml and resolves when replacement therapy is prescribed (Levina L.I.).
In addition, it should be remembered that with hypothyroidism there may be phenomena of intoxication with cardiac glycosides due to a decrease in their metabolism in the liver and a decrease in hepatic blood flow.
A reduction or disappearance of cardiovascular disorders in patients with hypothyroidism has been proven when adequate hormone replacement therapy is used (Starkova N.T.). Thus, Japanese researchers studied the dynamics of the thickness of the walls of the common carotid artery a year after normalization of the level of thyroid hormones under the influence of T4 intake and found a decrease in their thickness to the values of healthy individuals. A decrease in vascular wall thickness correlated with a decrease in total cholesterol and LDL cholesterol levels (Naggasaky T.).
- dyspnea.
- sleep disorders;
- nervousness;
- weight loss;
- increased sweating;
- increased frequency of urination;
- diarrhea;

Diagnostics
Drug therapy

Lifestyle correction
- eliminate alcohol and smoking;
View full version: Tachycardia, hypothyroidism.
You still have subclinical hypothyroidism - and everything related to manifest hypothyroidism has nothing to do with you
You do not have a ticket for one disease - but there is undoubtedly a pronounced desire to multiply entities unnecessarily
You have a strange habit of asking questions, not caring about the answers - what does this give you?
Perhaps you have a combination of several problems - what force is preventing the doctor from looking at you?
It may turn out that you have signs of adrenal insufficiency or evidence of celiac disease
Let's try again: You misunderstood what the doctor said. Or rather, what the doctor should have said. And he should have said the following:
Outside of a planned pregnancy, it is not necessary to treat subclinical hypothyroidism
With subclinical hypothyroidism, there may be tachycardia, but this does not mean that it is CAUSED BY IT
Correction of tachycardia (as well as additional clarification of its causes) is carried out regardless of the fact of hypothyroidism.
Even if you bring a carload of bricks (yoda), the house will not be built on its own
What was wrong with that answer?
A question arose about when is the best time for me to take a TSH test.
My chronology was like this:
1) I took thyroxine 50 mcg for 3 months (my weight is now 60 kg, height 187 cm);
2) decided to go to an endocrinologist due to the lack of improvement. He stopped thyroxine and prescribed iodine 200 mcg/day;
3) I have been taking iodine in this dosage for about 4 months.
I was told that TSH control would be done in 6 months. And I had a question, if I take a TSH test now, it will show my consequences of taking thyroxine along with iodine, i.e. will the result be confusing (it will be unclear what gave what)?
Second question: I read that if you have hypothyroidism, it is not advisable to take beta-blockers because they have an antithyroid effect. Then how can I relieve tachycardia? Only betaloc helps more or less.
Third question: what drugs can distort the TSH analysis, which is not recommended to be taken in the coming days, before taking the test.
Fourth question: is it worth taking T4 and T3 together with TSH? I ask because the cost is much more expensive, but is it necessary?
Thank you in advance!
Oh, yes, and another question that seems to follow from all of these (I myself can’t figure it out): “If tachycardia is caused by hypothyroidism, then how long after taking thyroxine at a dosage of 1 mcg/1 kg of body weight does an improvement in well-being occur, i.e. e. disappearance of tachycardia? I note that I took thyroxine for about 3 months, was it worth it to continue? Only after these 3 months I didn’t do a TTG.
Not true. I have already provided a link to the document that I prepared in advance. If necessary, I can even send you my photos, just give me some advice please. If necessary, I will post the results of the examinations that I completed. Here is the content of this document:
Disease history
Complaints: tachycardia at rest with heart rate 120 (especially in a standing position), poor heat tolerance, physical. exercise, heavy meals.
Before illness: height 187, body weight 64-66 kg.
[Early 2012] In the period from 2011 to 2012, I was engaged in physical education. Since 2012, I suddenly felt unwell (weakness, dizziness, shaking) after intensive skiing in cold weather (I was dressed quite lightly).
The temperature remained at 37.2 for 1.5 (one and a half) years;
severe weakness, dizziness;
strange attacks similar to panic attacks with trembling of the limbs, darkening of the eyes with great weakness and trembling;
sometimes pressing, aching, dull pain in the region of the heart;
enlarged lymph node in the armpit (+ redness of the skin in this area with itching and tingling).
After a year and a half, the body temperature became normal, periodically rising to 37.2.
Body weight 72 kg (kept at this level for half a year);
slight swelling of the limbs;
constant, non-episode tachycardia appeared at rest, especially in a standing position 120 beats/min; lying down, the pulse drops to 60-90 beats/min, but sometimes there were attacks of tachycardia while lying down with a heart rate of up to 120;
lack of air.
Since then, I have been taking a beta blocker (Betaloc) at a dose of 12.5-20 mg, enough for 1 day.
October, November (2 months) taking l-thyroxine 50 mcg/day without improving health.
December - to present iodine intake 200 mcg/day.
[Now] (as of April 2016) Weight 60 kg. Heart rate in a standing position is up to 120 beats/min, with simple walking or low-intensity work while standing 130-150 beats/min. Lack of air, yawning, fever. Tachycardia increases after eating food (especially hot food) and in hot weather, in a warm room. In the cold, manifestations decrease sharply. Shaking. Periodic extrasystole (the heart beats once, twice, arrhythmically). Sometimes the heart rhythm is completely arrhythmic with strong contractions.
The following examinations and analyzes were carried out:
2012
For oncology (Hodgkin's disease) - absent.
During this period, according to the KLA, hemoglobin is reduced
120.
He underwent a course of antibiotics to treat possibly hidden pneumonia.
2014
Echocardiography - within normal limits.
2015
ECG, daily Holter - within normal limits;
Ultrasound of the thyroid gland (summer 2015) - isoechoic node right lobe 6x4mm;
UAC - not normal ( low platelets 138 and high hemoglobin 187). Repeatedly (after 3 months) hemoglobin 164, platelets 180, ESR 1-2;
Blood tests for thyroid hormones are not normal (several tests): ranges of values at different periods of time TSH 10.24 - 9.0 -, 7.0 - 5.25; T4sv 18-10.5; T3sv - 6.
Blood test for RF, CRP, ASL-O - normal;
OAM - norm;
Daily total metanephrines in urine are normal;
Ultrasound of the hepatobiliary system is normal;
Throat smear (ENT) is normal;
MRI of the head is normal. There is no blood flow in the right VA, and the left VA is reduced. There are sinus cysts;
2016
Ultrasound of the thyroid gland (January 2016) - a hypoechoic node with unclear contours in the right lobe, 6x4 mm;
TSH (April 2016) - 4.52.
Relationship between heart tachycardia and thyroid gland
Some thyroid diseases are accompanied by the development of cardiac pathologies. One of them is tachycardia. The thyroid gland is one of the most important regulators of all processes occurring in the body, and malfunctions in its functioning negatively affect all organs and systems, but the heart muscle suffers the most.

Thyroid diseases are very common ailments in people of any gender and any age, and in order to prevent the development of severe pathologies, it is necessary to undergo a timely examination by a qualified specialist.
How does it affect the heart?
The connection between the work of the thyroid gland and heart contractions is obvious - the speed of the heartbeat depends on its work. The thyroid gland produces hormones that are very important for the balanced functioning of the body. With the help of thyroid hormones, not only all vital systems of the body are regulated, but also the organs are supplied with oxygen. In this regard, if there are disorders in the thyroid gland and it works at a reduced rhythm, thyroid hormones are synthesized in insufficient quantities, which provokes weakness and decreased heart rate. Conversely, when a goiter develops and the gland works at an accelerated pace, the pulse quickens, that is, tachycardia occurs.
Increased synthesis of hormones also occurs during inflammation in the gland, as well as in the presence of various formations that are hormone-dependent and produce hormones. In a person with problems in the functioning of this endocrine organ with a rapid heartbeat, the body is constantly in a stressful state, which increases the risk of developing dangerous cardiac pathologies that can lead to death.

Increased heart rate and thyroid function are related in this way. The heart muscle contracts under the influence of impulses, but with thyroid diseases (in particular hyperthyroidism), hormones that are produced in large quantities generate these impulses in a random order, which naturally affects the heart. So it starts beating faster. With hypothyroidism, bradycardia develops, that is, the heart rate decreases.
It must be said that the treatment of both tachycardia and bradycardia developing against the background of thyroid diseases is not complicated, but it is important that it is prescribed by an experienced doctor.
General symptoms of thyroid dysfunction
Symptoms that may indicate a malfunction of an important endocrine organ are the following:
- increase or decrease in body weight with a normal diet and constant physical activity;
- elevated cholesterol levels;
- chilliness or excessive sweating;
- intolerance to high or low temperatures;
- rapid or decreased heartbeat;
- muscle pain;
- diarrhea or constipation;
- insomnia;
- irregularities in the menstrual cycle;
- nervousness;
- depressed and lethargic state;
- swelling;
- dryness skin and hair loss.
All these symptoms are common, and it is impossible to make a correct diagnosis based on their presence alone.
There are many thyroid diseases, and each of them has its own individual symptoms. For example, with oncological processes in the gland, a person develops hoarseness in his voice, The lymph nodes increase, patients complain of difficulty swallowing and pain in the throat area.
With hypothyroidism, symptoms depend on the patient’s age, the degree of hormonal deficiency and the duration of the disease. In newborns, symptoms of hypothyroidism may be completely absent, and in children under 2 years of age, a clear symptom of thyroid hormone deficiency is short stature, mental retardation and learning difficulties.
Adults with hypothyroidism complain of excess weight, constipation, hair loss, a constant feeling of cold and dry skin. Women may experience reproductive dysfunction and disruptions in the menstrual cycle.
If a woman with hypothyroidism becomes pregnant, she has an increased risk of miscarriage, anemia, increased blood pressure, and possible premature birth. A child born to a woman with hypothyroidism may be delayed in mental and physical development and be underweight at birth.
As for older people, hypothyroidism is accompanied by deterioration of hearing and memory, and depression is possible. Many people mistake these symptoms for age-related changes.
The symptoms of hyperthyroidism also largely depend on the age and duration of the disease. In this case, patients develop tachycardia, nervousness, sharp weight loss, shortness of breath and sweating. In older people, hyperthyroidism is accompanied by arrhythmia and heart failure, and frequent attacks of angina are possible.

With inflammatory processes in the gland, patients experience weight gain, drowsiness, deepening of the voice and a feeling of presence foreign body in the throat. As the disease progresses, hair loss, chilliness, constipation and dry skin may appear.
A goiter or an increase in the size of the gland is accompanied by difficulty breathing or problems with swallowing; patients can visually see an increase in the volume of the neck.
Diagnosis of diseases

It is imperative to understand that tachycardia can be not only accompanying symptom at functional disorders thyroid gland, but also independent and very dangerous disease. For the diagnosis to be correct, the following methods are necessary:
- Oral inquiry. The doctor asks questions about the symptoms and determines the presence of disturbances not only in the functioning of the heart, but also nervousness, weakness and psychological disorders.
- ECG. If tachycardia is caused by disturbances in the functioning of the thyroid gland, then in most cases this analysis does not reveal pathologies in the heart (in the early stages of the disease, of course).
- EchoCG. If a patient is suspected of having hyperthyroidism, this test shows the presence of left ventricular hypertrophy.
- Ultrasound of the endocrine organ can visualize the presence of formations in the gland, inflammation or other pathological changes.
- Laboratory blood tests for thyroid hormones indicate malfunctions of the organ and explain the reasons for the development of tachycardia. In this case, it is advisable to donate blood after 10 pm, since it is at this time that the gland is most active.
Treatment of pathology
In order for the treatment of tachycardia for thyroid diseases to be effective, it is necessary to identify the cause of the disease and begin to eliminate it. As mentioned above, treatment of cardiac arrhythmia caused by pathological processes in the thyroid gland is not difficult, the main thing is to donate blood for hormones and, depending on the results, select therapy.
Naturally, all medications must be prescribed by a doctor, taking into account the patient’s age, duration of the disease, test results, the presence of other ailments and other factors.
For any dysfunction of the thyroid gland, hormonal drugs, but to improve the functioning of the heart muscle, patients are prescribed sedatives - motherwort tincture, Corvalol, Valerian, Valocordin, Novo-passit and others. The doctor may also recommend taking antiarrhythmic drugs - Adenosine, Verapamin, and so on.

In addition, therapy with physiotherapy or traditional methods of therapy is recommended, but they must be discussed with the attending physician. In especially severe cases, if the disease cannot be treated conservative treatment, surgery may be prescribed. Tachycardia and the thyroid gland have a direct connection, but we must not forget that the cause of rapid heartbeat may not lie in diseases of the endocrine organ, so consultation with a doctor is mandatory.
Traditional therapy
First of all, in case of tachycardia caused by disorders in the thyroid gland, you should give up coffee, strong tea, smoking, fatty foods, salty and spicy foods. Meals should be regular, balanced and healthy. Overeating must be avoided, as this phenomenon can provoke unwanted attacks. It is useful to include natural honey, bran, fruits and vegetables in your diet. It is very important to stop being nervous and experiencing emotional overload.
To lower your heart rate, you can use non-traditional treatment methods. Very effective means is oat juice. You need to squeeze the juice from the above-ground part of the plant and drink it half a glass 2-3 times a day. This remedy is especially indicated for those whose tachycardia is regularly accompanied by high blood pressure.
Hawthorn is a well-known remedy for treating heart ailments. For tachycardia caused by a malfunction of the thyroid gland, it is very useful to drink tea with these fruits. In addition, it is useful to add motherwort herb to tea.
Blue cornflower also copes well with tachycardia. For a glass of boiling water, you need to take a teaspoon of flowers, leave for an hour, then filter and drink half a glass several times a day.
If tests show too thick blood, then sweet clover can help. It has a blood thinning effect. Sweet clover can be combined with other herbs and drunk as tea. If you drink this remedy for six months, your blood pressure will stabilize and the attacks of tachycardia will disappear.
Instead of tea, you can brew lemon balm; it also perfectly relieves attacks of tachycardia. if you have tea mushroom, then it can be infused not only with regular tea, but also with medicinal herbs. Use heather, foxglove, motherwort, black cohosh. Take all ingredients in equal proportions, pour boiling water and leave to steep overnight. Then add honey and pour over the mushroom. After a week, the healthy drink is ready for use. Drink 100 grams of it before meals.
Honey and lemon are often used in the treatment of tachycardia, so it is recommended to prepare a tasty treat from a mixture of honey, almonds and lemon. Half a kilo of lemon and 30 peeled almonds will require half a kilo of honey. Finely chop the lemon and crush the nuts. Mix everything with honey and consume 1 tbsp. l. 2 times a day.
Prevention of heart pathology
To prevent complications in the form of heart pathologies from occurring in the event of problems with the thyroid gland, it is important to begin treatment of ailments at the very beginning of their development. Patients should undergo regular examinations, avoid emotional and physical overload, and take all medications recommended by the attending physician.
Diseases of the thyroid gland can be successfully treated with medications; they are easy to identify, so you should not put off treatment for a long time. In order for the heart and the entire body to work correctly and not give any failures, you need to carefully monitor the condition of the main endocrine organ, and promptly consult a doctor to eliminate pathological manifestations.
Tachycardia due to hypothyroidism
First of all, indicate the results of tests for thyroid hormones with delivery dates, units of measurement and standards in your laboratory.
Also attach to the message a photo of the protocol (description) of an ultrasound examination of the thyroid gland in good resolution.
How long have you been taking Euthyrox at a dosage of 75 mcg?
Sincerely, Nadezhda Sergeevna.
If you did not find the information you need among the answers to this question, or your problem is slightly different from the one presented, try asking an additional question to the doctor on the same page, if it is related to the topic of the main question. You can also ask a new question, and after a while our doctors will answer it. It's free. You can also search for the information you need in similar questions on this page or through the site search page. We will be very grateful if you recommend us to your friends on social networks.
Medical portal 03online.com provides medical consultations via correspondence with doctors on the website. Here you get answers from real practitioners in your field. Currently, on the website you can get advice in 45 areas: allergist, venereologist, gastroenterologist, hematologist, geneticist, gynecologist, homeopath, dermatologist, pediatric gynecologist, pediatric neurologist, pediatric surgeon, pediatric endocrinologist, nutritionist, immunologist, infectious disease specialist, cardiologist, cosmetologist, speech therapist, ENT specialist, mammologist, medical lawyer, narcologist, neurologist, neurosurgeon, nephrologist, oncologist, oncourologist, orthopedist-traumatologist, ophthalmologist, pediatrician, plastic surgeon, proctologist, psychiatrist, psychologist, pulmonologist, rheumatologist, sexologist-andrologist, dentist, urologist, pharmacist, herbalist, phlebologist, surgeon, endocrinologist.
We answer 95.05% of questions.
Features of the manifestation and treatment of tachycardia provoked by thyroid diseases
Violations heart rate can develop against the background of certain diseases of the thyroid gland, since it is involved in the activities of various body systems. The connection between these pathologies can be revealed through a comprehensive examination. Therapy must be prescribed based on its results.
Can thyroid disease provoke tachycardia?
Normal functioning of the thyroid gland is important for the functionality of various body systems. Organ dysfunction causes changes, including in the activity of the heart.
Heart rate is related to the condition of the thyroid gland. It synthesizes many hormones that regulate the functioning of the body and provide tissues with oxygen. Hormonal levels rise and heart rate increases. This often occurs against the background of neoplasms or inflammatory process.
The development of tachycardia is due to the constant connection between the heart and the thyroid gland. An increase in hormonal levels is reflected in the sinus node, which is located in the right atrium. It generates electrical impulses that cause myocardial contractions. At high hormonal levels, they reproduce chaotically, affecting the heart. As a result, it contracts faster, the heartbeat quickens, and tachycardia occurs.
With thyroid diseases, metabolic processes can accelerate. This causes the heart muscle to contract intensely, creating chronic stress. Such changes can result in heart failure, which can be fatal.
Against the background of thyroid disease, tachycardia can be a reflex phenomenon. An increased heart rate in such cases is a reaction to an attack of severe pain.
Symptoms of tachycardia in diseases of the thyroid gland
If tachycardia is caused by disruptions in the functioning of the thyroid gland, disorders can be recognized by the following symptoms:
- heart rate exceeds normal (upper limit 90 beats) and may increase to 140 beats per minute;
- during physical and mental stress, heart contractions accelerate to 160 beats per minute and above, such indicators are a critical level;
- heart rate does not depend on body position and whether a person is sleeping or awake;
- there is pain in the chest;
- The heartbeat is felt by a person: it radiates to the neck, abdomen, head;
- dyspnea.
Such signs of tachycardia simultaneously overlap with symptoms indicating pathology of the thyroid gland. The patient can observe:
- sleep disorders;
- nervousness;
- weight loss;
- increased sweating;
- increased frequency of urination;
- diarrhea;
- menstrual irregularities.
The signs of thyroid disease are quite general, so pathology in this area can only be confirmed after a comprehensive examination. Tachycardia can be caused by various diseases of this organ, and each has its own specific symptoms.
When diagnosing tachycardia against the background of thyroid pathologies, signs of systolic hypertension are often detected. In this case, an increase in pressure is observed only in the systolic parameter; in diastole, the indicators remain normal or change downward. Systolic hypertension is triggered by an increase in cardiac output and stroke volume, to which vascular system cannot adapt.
The severity of symptoms depends on the form of hyperthyroidism (hyperthyroidism):
- If it is mild, then the main manifestations are neurotic in nature. The heart rate in this case increases to a maximum of 100 beats per minute. Slight weight loss is possible.
- For pathology medium degree severity, heart contractions can increase to 100 beats per minute. A person's body weight decreases noticeably. Weight loss in a month can be up to 10 kg.
- A severe form of hyperthyroidism is called visceropathic or arrowroot. The disease progresses to this stage in the absence of proper treatment. This form provokes persistent heart rhythm disturbances. Tachycardia can lead to atrial fibrillation and cause heart failure. This threatens accelerated breakdown of hormones and subsequent acute adrenal failure. In severe hyperthyroidism, weight loss is significant. Cachexia is possible when the body is extremely exhausted. This condition is accompanied by changes in a person’s mental state, the activity of physiological processes decreases sharply.
The severity of symptoms of thyroid pathologies also depends on age. In children, signs of the disease may be absent or expressed by short stature, mental retardation, difficulty in learning. These disorders often negatively affect the state of the nervous system, which can serve as a trigger for the development of tachycardia.

Diagnostics
Diagnosis of any disease begins with taking an anamnesis. Symptoms of tachycardia are more often alarming, and pathology of the thyroid gland is detected during the examination. At the initial stage, the specialist is interested in all the symptoms accompanying increased heart rate, the connection of existing disorders with sleep and mood.
During the examination, pulse and blood pressure must be measured. Further diagnosis is carried out using clinical and instrumental studies:
- Blood test for hormones. Such a study will show the amount of thyroid hormones. The test results are most accurate when blood is drawn in the evening, since maximum thyroid activity occurs at 10-11 pm.
- Electrocardiogram. This technique is designed to test the heart. Based on its results, it is impossible to suspect a pathology of the thyroid gland and identify its connection with tachycardia.
- Echocardiography. This study reveals left ventricular hypertrophy. This sign indicates hyperthyroidism.
- Ultrasound examination of the gland. Scanning is necessary to identify pathological changes in the thyroid gland, inflammation, and neoplasms. If necessary, a fine-needle biopsy of the gland can be performed under ultrasound guidance.
- Scintigraphy. Such a study may show reduced metabolic activity of cardiomyocytes. These changes can be small-focal or diffuse in nature.
- Additionally, an x-ray may be performed. When tachycardia is caused by hyperthyroidism, both ventricles are enlarged.
Features of treatment of tachycardia
If tachycardia is caused by a disease of the thyroid gland, then the goal of treatment is to eliminate the primary disease or relieve its manifestations.
Drug therapy
Treatment with drugs is prescribed based on the results of a hormone test. Required medicines to suppress organ function in order to normalize the production of hormones. In some cases, treatment is required for life.
Drugs that suppress thyroid function are prescribed exclusively by a specialist. The dosage is determined individually and calculated depending on the level of hormones in a particular patient.

To reduce heart rate and myocardial contractility, beta-blockers are used. More often, treatment is performed with Propranolol, Anaprilin, Inderal. These drugs are non-selective β-blockers. Such drug therapy is prescribed taking into account individual sensitivity to drugs and the results of physiological tests (performed under the control of an electrocardiogram).
In case of tachycardia due to thyroid disease, it is necessary to improve the functioning of the heart muscle. For these purposes, they resort to sedatives. Provide good effect herbal preparations: motherwort tincture, valerian preparations, Persen, Novo-Passit.
If tachycardia due to pathologies of the thyroid gland is accompanied by arterial hypertension, then it is advisable to prescribe calcium antagonists. Such drugs, like beta-blockers, are classified as antiarrhythmic drugs. Among the calcium antagonists, Isoptin, Finoptin, and Corinfar are most often used.
Lifestyle correction
When tachycardia occurs against the background of thyroid pathologies, it is necessary to adhere to a certain lifestyle. Several recommendations should be followed:
- eat regularly and balanced;
- overeating is prohibited, portions should be small;
- give up caffeine and strong tea;
- reduce the level of table salt in the diet;
- eliminate alcohol and smoking;
- avoid emotional overload and stress.
Some diseases of the thyroid gland can lead to the development of tachycardia. The mechanisms of development of disorders may vary, but in any case the patient needs competent treatment. The features of therapy can be determined only after a full diagnosis of the state of the endocrine and cardiovascular systems.
Irina TERESCHENKO, prof.,
Perm State Medical Academy
Practitioner's Notes
At the XI International Endocrinology Congress, held recently in Sydney (Australia), special attention was paid to cardiopathy caused by thyroid pathology. Of course, this problem is becoming more and more urgent as the prevalence of this pathology increases. Recently, more attention has been paid to thyroid disorders on the border between normal and pathological: subclinical thyrotoxicosis and subclinical hypothyroidism. Their high prevalence has been proven, especially in older people, mainly in women. A number of regions have introduced screening for subclinical forms of thyroid disease in older age groups. A disturbance in the content of thyroid hormones in the body, even a slight increase or decrease, causes pathology of the cardiovascular system.
Heart with subclinical hypothyroidism
Subclinical hypothyroidism is a pathological condition characterized by normal level total and free thyroxine (T4) and increased level thyrotropin (TSH), or hypersecretion of TSH, in response to the administration of thyrotropin-releasing hormone (THH).
It should be remembered that in some cases, even with manifest hypothyroidism, especially in the elderly, there is no increase in TSH levels. This feature is due to environmental problems (environmental pollution with lead, cadmium, carbon monoxide, etc.), exposure to drugs (rauwolfia, clonidine, etc.), and protein deficiency in food. It has also long been noted that in the zone of iodine deficiency, the synthesis of TSH by the pituitary gland is reduced.
Cardiac “masks” of subclinical hypothyroidism:
- persistent hypercholesterolemia, atherogenic dyslipidemia;
- atherosclerosis;
- arrhythmias (sinus bradycardia or tachycardia, polytopic extrasystole, paroxysms of atrial fibrillation and flutter, sick sinus syndrome);
- cerebrovascular disease;
- arterial hypertension;
- mitral valve prolapse (MVP) (and/or other valves), hydropericardium
Subclinical hypothyroidism includes endemic goiter (EG). It has long been known that patients with EZ develop cardiac complaints, the sonority of heart sounds and heart rhythm may change. However, these changes in the activity of the cardiovascular system were previously considered to be mild and caused by autonomic dysregulation. The widespread use of ultrasound examination of the heart has revealed the frequent development of prolapse of the mitral valve or other valves in EZ and other cases of subclinical hypothyroidism.
Mitral valve prolapse is the systolic protrusion of one or both mitral leaflets into the cavity of the left atrium above the level of the mitral annulus. In this case, a violation of the closure of the valves with the development of mitral regurgitation does not always develop. More than 50 diseases are known in which MVP can develop. However, EZ and hypothyroidism as etiological factors of MVP have not received due attention even in the literature of recent years. Meanwhile, even an insignificant deficiency of thyroid hormones in the body causes serious metabolic disorders, including dystrophic changes in the heart, accompanied by a decrease in the intensity of oxidative phosphorylation, a slowdown in protein synthesis, a decrease in oxygen uptake by the myocardium, and electrolyte shifts. Both the contractile myocardium and the stroma are affected. Creatine phosphate is deposited in cardiomyocytes and so-called myocardial pseudohypertrophy occurs. In the heart, as in other tissues, acidic glycosaminoglycans are deposited, leading to mucous edema of the myocardium and stroma.
With EZ and hypothyroidism, the autonomic system is involved in 100% of cases. nervous system. Autonomic dystonia is characterized by vagal hypertonicity, that is, parasympathetic autonomic dysregulation of the heart occurs. As a rule, MVP in patients with EZ and subclinical hypothyroidism has a “silent” course: the number of heart contractions and cardiac configuration remain normal, but in most cases there is a decrease in one or both tones. The classic manifestations of MVP - mesosystolic, less often protosystolic, or late systolic click, precordial “click” (auscultatory phenomenon of resonance of the mitral leaflet) are not recorded. When analyzing electrocardiograms, deviations from the norm (sinus bradycardia, slowing of impulse conduction in different parts of the myocardium, decreased voltage of the waves, especially the T wave) are observed in 80% of cases, but are not of a regular nature.
Ultrasonography has established that against the background of latent hypothyroidism, MVP often occurs, in some cases combined with prolapse of the tricuspid and/or aortic (extremely rare - pulmonary) valve. The displacement of the mitral valve leaflets into the atrium cavity reaches 3-7 mm; this is the I or II degree of MVP. Regurgitation is found only in isolated cases; The diastolic opening of the mitral valve is not impaired, the volume of the left atrium is normal and, therefore, serious hemodynamic disturbances do not develop. Nevertheless, MVP can be called an important diagnostic symptom of EZ and subclinical hypothyroidism.
III degree prolapse, that is, more than 9 mm, is not typical for patients with subclinical hypothyroidism. In these cases, even in the presence of EZ, one should look for other causes of MVP.
Despite the absence of regurgitation and hemodynamic disturbances in patients with EZ with MVP, the risk of prolapse complications remains. Typical complications of MVP are infective endocarditis, thromboembolism, and sudden death. Therefore, it is relevant to develop methods for the treatment of MVP in patients with EZ and subclinical hypothyroidism.
It is known that for the treatment of MVP, β-blockers are used to suppress the increased contractility of the left ventricular myocardium during MVP, as well as to increase its volume and prevent arrhythmias. It should be emphasized that β-blockers are contraindicated in cases of hypothyroidism, since they have an antithyroid effect and increase hypothyroidism. In addition, parasympathicotonia also serves as a contraindication to the use of these drugs in such patients. Systematic replacement therapy with thyroid hormone drugs reduces or completely eliminates MVP in patients with EZ and subclinical hypothyroidism. On the contrary, without correction of thyroid insufficiency, prolapse of other valves may appear and regurgitation may increase.
Another echocardiographic finding in patients with subclinical hypothyroidism, including patients with EZ, may be hydropericardium, which is asymptomatic. Typically, the effusion is localized in the apex and along the right contour of the heart.
Heart with subclinical hyperthyroidism
Subclinical hyperthyroidism is a condition in which the concentration of TSH (without pituitary insufficiency) in the blood serum decreases, while the levels of thyroid hormones in the serum remain within normal limits.
Before making a diagnosis of subclinical hyperthyroidism, especially in the elderly, it is necessary to repeatedly determine the TSH level over time over several weeks, since a decrease in the basal TSH level can be observed with various non-thyroid diseases, depression, taking certain medications, etc. The true prevalence of subclinical hyperthyroidism in our country has not yet been studied. In England it is about 10% in women, in other countries it varies from 0.5% to 11.8%.
The causes of subclinical hyperthyroidism are different: it is a euthyroid variant of Graves' disease, a toxic adenoma of the thyroid gland, a consequence of the destruction of thyrocytes in subacute or chronic thyroiditis, as well as insufficient adequate treatment of overt hyperthyroidism. Most common cause lowering TSH levels is taking thyroxine (drug-induced subclinical hyperthyroidism). It often occurs during pregnancy. Gestational hyperthyroidism, caused by increased levels of human chorionic gonadotropin during developing pregnancy, can also often be subclinical. Iodine-Basedowism, high iodine consumption with imperfect mass prevention of EZ in many cases occurs as subclinical hyperthyroidism. For the clinician, it is important to answer the question whether subclinical hyperthyroidism affects health, and primarily the cardiovascular system, or is it just a laboratory finding.
The effect of thyroid hormones on the circulatory system is well known. They play an important role in regulating energy metabolism in the body. Their effect on mitochondrial processes in cells, including cardiomyocytes, has recently been clarified. Thyroid hormones regulate the lipid composition of mitochondrial membranes, the content of cytochromes and cardiolipins in cells, etc., ultimately stimulating cellular respiration. These effects are divided into short-term (several hours) and long-term (several days). In subclinical hyperthyroidism, these processes are disrupted. Thus, when examined as part of the Framingham Study, patients with a TSH level of less than 0.1 milliU/L were found to have a significantly higher incidence of atrial fibrillation after 10 years and a significantly increased mortality rate.
The following clinical cardiac symptoms are characteristic of subclinical hyperthyroidism:
- tachycardia,
- shortening of systolic intervals,
- increase in left ventricular stroke volume,
- diastolic abnormalities (decreased diastolic filling)
Should subclinical hyperthyroidism be treated? Currently, there is no evidence-based medicine assessment yet. It has been empirically shown that the use of β-blockers improves pulse, reduces atrial fibrillation, and diastolic dysfunction in patients treated with thyroxine.
If subclinical hyperthyroidism is a variant of Graves' disease, then the effectiveness of β-blockers is currently questioned (M. Niels, H. K. Yde, N. Soren et al., 1998).
The question of whether such patients should be treated with thyreostatics has not been resolved. “Wait and watch,” especially if there are no obvious disturbances in cardiac function and bone metabolism, is one point of view. But since subclinical hyperthyroidism in many cases can quickly progress to overt clinical form, then there are many supporters of the active use of thyreostatics. Obviously, the decision must be made individually.
Heart with manifest hypothyroidism and manifest thyrotoxicosis
The terms “myxedematous (hypothyroid) heart” and “thyrotoxic heart”, which are currently used to designate myocardial damage in manifest hypothyroidism or manifest thyrotoxicosis, were first proposed by H. Zondek at the beginning of the twentieth century. Let us consider the pathogenetic mechanisms of hypothyroid and thyrotoxic heart.
| Pathogenesis of hypothyroid heart | Pathogenesis of thyrotoxic heart |
|
|
The most significant complications that threaten the lives of patients with hypothyroidism and thyrotoxicosis are caused by pathological changes in the cardiovascular system: rhythm and conduction disturbances, cardialgia, arterial hypertension, myocardial dystrophy, circulatory failure.
Arrhythmias in thyroid pathology
The idea that bradycardia is inevitable with hypothyroidism has long been outdated. Indeed, sinus bradycardia is a characteristic, but not an absolute clinical sign of hypothyroidism, including myxedema: the tachysystolic form of atrial fibrillation and flutter is often observed, usually in the form of paroxysms. The alternation of such paroxysms with bradycardia is mistakenly taken for sick sinus syndrome as a consequence of coronary artery disease. A thorough examination of the patient is required, including electrophysiological and hormonal studies. Treatment with antiarrhythmic drugs in such cases is not only useless; Amiodarone, Sotalex and other antiarrhythmics aggravate hypothyroid arrhythmia.
There is an interesting description in the literature of ventricular flutter-fibrillation in myxedema, eliminated by thyroid hormones without antiarrhythmic therapy (A. Gerhard et al., 1996). Conduction disturbances in different parts of the heart are also common in hypothyroidism.
In a thyrotoxic heart, persistent sinus tachycardia is observed. Heart rate does not depend on either emotional or physical activity. Tachycardia does not decrease during sleep. In severe cases of the disease, patients develop a tachysystolic form of atrial fibrillation. Treatment with amiodarone and saluretics provokes atrial fibrillation. Extrasystole in thyrotoxicosis is rare. Its appearance is associated not with thyrotoxicosis, but with a previous heart disease.
Thyroid diseases and arterial hypertension
Arterial hypertension is observed in both hypothyroidism and hyperthyroidism, but the pathogenetic mechanisms are different.
Arterial hypertension in hypothyroidism is aggravated by the associated atherosclerotic process. In this case, its course does not differ from the course of essential hypertension, but partial or complete refractoriness to antihypertensive drugs develops.
Arterial hypertension in thyrotoxicosis is called high cardiac output syndrome, while left ventricular hypertrophy is usually absent. The recently discovered peptide adrenomedullin has very pronounced vasodilator activity. Its participation in reducing diastolic blood pressure in patients with thyrotoxicosis has been proven. High cardiac output syndrome may develop into hypertension. If arterial hypertension in a patient persists for several months after normalization of thyroid function, this case should be considered as a transition to essential hypertension and conventional antihypertensive therapy should be carried out.
Heart failure in hypothyroid and thyrotoxic heart
In hypothyroidism, despite pronounced dystrophic changes in the myocardium, heart failure occurs extremely rarely (in myxedema with a long history of the disease). This is explained primarily by a decrease in the need for peripheral tissues for oxygen, as well as vagotonia.
In thyrotoxic heart, a decrease in myocardial contractile function and the development of heart failure depends on the severity of the disease. Shortening of diastole leads to depletion of the reserve capacity of the myocardium. The contraction power of both ventricles decreases, which is the result of significant fatigue of the heart muscle due to developing myocardial dystrophy. At the same time, total peripheral resistance decreases and pulmonary resistance increases. Increased pressure in pulmonary artery occurs due to reflex narrowing of the pulmonary arterioles (Kitaev reflex). Hemodynamic disorders in thyrotoxicosis lead to the fact that the left ventricle of the heart operates under conditions of isotonic hyperfunction (volume load), and the right ventricle operates under conditions of mixed type hyperfunction (volume and resistance load).
Heart failure in thyrotoxicosis develops predominantly of the right ventricular type. At the same time, it can be aggravated by the developing insufficiency of the tricuspid valve with regurgitation of blood into the right atrium. MVP occurs frequently in thyrotoxicosis, but does not significantly affect hemodynamics, although in some cases signs of left atrial hypertrophy can be found on the ECG (S.B. Shustov et al., 2000).
| ECG changes in thyrotoxicosis | ||
| with a mild course of the disease | with moderate thyrotoxicosis or long duration diseases | for severe thyrotoxicosis |
|
|
|
Differential diagnosis of thyrotoxic heart and rheumatic carditis
Experience shows that heart changes during the manifestation of thyrotoxicosis are often mistakenly interpreted as manifestations of primary rheumatic carditis, especially if the symptoms appeared after a tonsillar infection. Shortness of breath, palpitations, heart pain, weakness, low-grade fever, prolongation of the PQ interval on the ECG are characteristic of both diseases. It is clear that antirheumatic therapy will not only have no effect, but may worsen the condition of patients.
The following clinical signs help in making the correct diagnosis: with thyrotoxicosis, patients are excitable, they have diffuse hyperhidrosis, warm palms, “Madonna” hand, persistent tachycardia, increased heart sounds, systolic arterial hypertension, and with rheumatic carditis, patients are lethargic, local sweating, hands the hands are cold, the tachycardia is inconsistent, intensifies after exercise, the 1st sound at the apex of the heart is weakened, blood pressure decreases.
Differential diagnosis of thyrotoxic heart and mitral valve disease
Diastolic murmur always indicates organic damage to the heart. Thyrotoxicosis is an exception: systolic and diastolic murmurs arise due to disruption of laminar blood flow in the cavities of the heart due to accelerated blood flow, decreased blood viscosity, and the addition of anemia. Auscultatory changes in the heart in patients with thyrotoxicosis are mistakenly interpreted as a sign of mitral disease. The mitral configuration of the heart, which appears in thyrotoxicosis due to increased pressure in the pulmonary artery (smoothness of the waist of the heart due to the bulging conus pulmonale) “confirms” the diagnosis.
Of course, sonographic examination of the chambers, cavities, and valve apparatus of the heart helps to avoid this kind of diagnostic errors. But even in patients with heart defects, it may be necessary to monitor TSH in the blood to confirm the diagnosis.
Differential diagnosis of thyrotoxic cardiopathy and ischemic heart disease
Diagnosis of thyrotoxicosis can be difficult in the elderly due to clinical similarities with coronary artery disease and atherosclerosis. Fussiness in behavior, sleep disturbances, hand tremors, increased systolic and pulse blood pressure, paroxysmal or permanent form of atrial fibrillation can be observed in both thyrotoxicosis and atherosclerosis. However, with thyrotoxicosis, the tachycardia is persistent, the heart sounds are increased even with atrial fibrillation, the level of cholesterol and LDL in the blood decreases, diffuse hyperhidrosis is expressed, hand tremors are small, a goiter, shiny eyes and other symptoms of thyrotoxicosis can be detected. These signs are uncharacteristic of atherosclerotic heart disease, and weakening of the 1st tone and hyperlipidemia will suggest coronary artery disease.
It should be taken into account that both diseases are often combined, thyrotoxicosis is layered on top of long-standing atherosclerosis. Since thyrotoxicosis can occur in elderly people without enlargement of the thyroid gland, it is necessary to monitor their TSH levels in the blood more often.
Treatment of hypothyroid heart
Eliminating hypothyroidism and achieving a euthyroid state gives undoubted success in the treatment of hypothyroid heart. The main drug for the treatment of hypothyroidism is thyroxine. Its average dose is 10-15 mcg/kg in children and 1.6 mcg/kg in adults; usually daily dose in women 75-100 mcg, in men 100-150 mcg. In young adult patients with hypothyroidism, the initial dose of thyroxine is 50-100 mcg/day. It is increased every 4-6 weeks by 50 mcg. In elderly patients, with ischemic heart disease and rhythm disturbances, the initial dose of thyroxine should not exceed 25 mcg/day. It is increased carefully under the control of general condition and ECG after 5-6 weeks. Treatment occurs under the control of TSH and thyroid hormones in the blood.
It should be remembered that many drugs, such as β-blockers, tranquilizers, central sympatholytics, amiodarone and sotalol, etc., can themselves cause drug-induced hypothyroidism.
Treatment of thyrotoxic heart
Elimination of thyrotoxicosis is the first condition for successful treatment of thyrotoxic heart. There are three types of treatment for Graves' disease: medication, surgery, and radioactive iodine therapy. Among the methods of conservative therapy, thyreostatic drugs (mercazolyl, or its analogues thiamazole, methimazole) are still used. Propylthiouracil is increasingly entering practice in the treatment of thyrotoxicosis. Although its dose is approximately 10 times higher than the dose of Mercazolil, it nevertheless has a number of advantages.
Propylthiuracil is able to bind tightly to blood proteins, which makes it suitable for the treatment of pregnant and lactating women. Its additional advantage is the ability to inhibit the conversion of T4 to T3. Compared to Mercazolil, a smaller amount of propylthiouracil penetrates into the placenta and breast milk. Along with the antithyroid effect, it also has an antioxidant effect, which is very important in the presence of oxidative stress in patients with thyrotoxicosis.
The question of the regimen of taking thyreostatics for Graves' disease must be resolved in two stages: first to achieve a euthyroid state, and then to carry out maintenance therapy to achieve long-term remission of this chronic autoimmune disease. The question remains debatable with what doses therapy with thyreostatic drugs should be started - with maximum doses, gradually decreasing, or with small ones. In recent years, there has been more and more support for the treatment of thyrotoxicosis with small doses of thyreostatics. Reducing the dose of thyreostatics reduces the number of side effects and does not weaken the antithyroid effect.
It should be noted that in patients with large goiters and/or high levels of T3 in the blood serum, small doses of thyreostatics cannot achieve a euthyroid state even after a long (more than 6 weeks) course drug treatment. Therefore, the tactics of drug treatment of thyrotoxicosis should be individual.
There is no single point of view on the tactics of maintenance therapy. There are fewer supporters of the use of high doses of thyreostatics in combination with thyroxine, according to the “block and replacement” principle, than supporters of minimal doses of thyreostatics sufficient to maintain a euthyroid state. Prospective studies, including a European multicenter study, have not shown any benefit from maintenance treatment with high doses of drugs. According to the results of surveys of both European and American specialists, 80-90% of endocrinologists believe that the course of maintenance therapy should be at least 12 months.
The question of the optimal duration of treatment remains open. It is believed that treatment can be recommended for 18 months, especially in patients who have antibodies to TSH receptors in their blood.
When carrying out treatment, it is necessary to remember the side effects of thyreostatics. Although hematological complications (agranulocytosis, aplastic anemia) develop rarely (in 0.17%-2.8% of cases), they are serious and can be fatal. It should be noted that agranulocytosis can develop with a low dose of thyreostatic drugs, and after a long period (12 months) after the start of their use.
Hepatotoxicity is often observed during treatment with thyreostatics, and the frequency of this pathology increases with increasing dosage of drugs. 10-25% of patients experience minor treatment side effects such as urticaria, itchy skin, arthralgia, gastritis, etc. These effects are clearly dose-dependent and require selection of an individual dose of thyreostatic for each patient.
The frequency of relapses of Graves' disease after a long course of maintenance therapy with thyreostatics, according to the observations of various authors, ranges from 2 to 35%. Currently, the opinion that combined therapy with thyreostatics and thyroxine significantly reduces the frequency of disease relapses has been revised; Prospective studies have not confirmed this. However, another 78% of Japanese doctors continue to use antithyroid drugs in combination with thyroxine (M. Toru et al., 1997). There are no clear criteria yet to predict the onset of remission of Graves' disease. However, the following factors may indicate the possibility of an unfavorable outcome of the disease: large goiter sizes, an initial high level of thyroid hormones in the blood, or a high titer of antibodies to TSH receptors.
A method for using thyreostatics in combination with cholestyramine has been developed. The latter reduces thyrotoxic intoxication by absorbing thyroid hormones in the stomach and intestines and preventing their reabsorption.
In many countries, combined treatment with thyreostatics and radioactive iodine is used for Graves' disease. This treatment is currently being tested because it is unclear whether thyreostatic therapy has an adverse effect on the effectiveness of subsequent radioactive iodine treatment. Transient hypothyroidism often develops after such treatment in patients with Graves' disease, and its development cannot be predicted in advance.
Surgery remains the fastest method of achieving a euthyroid state compared with thyroid drugs or radioactive iodine and, in addition, as shown by a randomized prospective study, this type of treatment is accompanied by the lowest relapse rate over the next two years. However, the risk of complications allows us to recommend performing strumectomies only in those surgical centers where there is sufficient experience. But even under this condition, the frequency of delayed development of severe hypothyroidism is at least 30% after 5 years, and subclinical hypothyroidism is even more common (up to 46% of cases), although in some patients it is cured spontaneously.
The issue of the optimal volume of surgical intervention for Graves' disease is still being debated. After subtotal thyroidectomy, delayed (5-10 years after surgery) relapses of thyrotoxicosis may develop in at least 10% of cases. Therefore, there have been many supporters of radical treatment of Graves' disease - total thyroidectomy. The need for constant replacement therapy with thyroid hormones in this case is a serious objection to this method of surgical treatment.
The use of cardiac glycosides in patients with thyrotoxicosis, even with severe shortness of breath, is a gross mistake. It is known that cardiac glycosides have a cardiotonic effect, cause an increase in cardiac systole, prolongation of diastole, a vagotropic effect, and a slowdown in conduction, in particular atrioventricular conduction. With thyrotoxicosis, there is a hyperkinetic type of hemodynamics, slowing of atrioventricular conduction, and therefore the use of cardiac glycosides is pointless. Resistance to these drugs in thyrotoxic hearts has long been noted. Refractoriness to antiarrhythmic drugs in patients with thyrotoxicosis is an indisputable fact. Amiodarone, which consists of 1/3 iodine, has a particularly harmful effect. There are descriptions in the literature of cases of the development of thyrotoxic crisis during treatment with amiodarone in patients with unrecognized thyrotoxicosis. Of course, with a thyrotoxic heart, it is necessary to prescribe drugs that improve metabolism in the myocardium: macroergs, vitamins, antioxidants, potassium and magnesium preparations.
Heart changes in thyroid cardiopathy are reversible if correction of thyroid function is started in a timely manner.
The attending physician individually determines how to take Eutirox for hypothyroidism, taking into account the age, characteristics of the patient, in accordance with the duration and nature of the disease.
Thyroid gland and its hormones
The thyroid gland, called the thyroid gland in the 17th century, is located in anterior section neck, next to it are the parathyroid glands. This small organ is a vulnerable place from the point of view of causing any injury or infection. The two lobes are connected by an isthmus, shaped like a shield. The gland, with its main endocrine function, is a participant in various processes of the body. Without the work of an organ, it is impossible to imagine the growth and development of any organism.
The main role of the thyroid gland, as it is popularly called, is the production of hormones:
- thyroxine;
- tyrosine;
- Iodine tyranine.
Thyroxine stimulates the growth of the body as a whole, increasing resistance to high temperatures. It is produced from the intrauterine stage of human development. Without it, growth in height, development of mental abilities, and stabilization of the immune system do not occur. Under the influence of hormones, protection is enhanced - cells are more easily freed from foreign elements.
The production of hormones is regulated by higher glands - the hypothalamus and pituitary gland. The pituitary gland produces thyroid-stimulating hormone, which causes the thyroid gland to increase not only the production of iodothyranine and thyroxine, but also activates the growth of the gland itself. The hypothalamus is the control center where nerve impulses arrive. It produces hormones that regulate the activity of the pituitary gland.
Thus, under the guidance of the hypothalamus, throughout the day, the thyroid gland produces up to 300 micrograms of thyroid hormones, which ensure the development and construction of the nervous system. When the amount of hormones is excessive or insufficient, the nervous system responds with excitability or depression.

Eutirox for hypothyroidism
Hypothyroidism is characterized by a decrease in the concentration of the hormone in the blood. Often hormonal deficiency is not detected for a long time, since the symptoms develop slowly and do not affect the condition general health, but occur under the masks of other diseases. With a chronic lack of thyroid hormones in humans, the metabolic processes, resulting in reduced energy and heat generation. The initial or obvious symptoms of hypothyroidism include:
- chilliness;
- loss of appetite with weight gain;
- drowsiness;
- dryness of the epidermis;
- poor concentration, lethargy;
- dizziness;
- depression;
- constipation;
- cardiovascular disorders.

For deficient thyroid function, so-called hypothyroidism, Eutirox, a synthetic analogue of thyroxine, is primarily indicated. This drug is used for replacement purposes. The drug belongs to the category of iodine regulators in the body.
Clinical experience and recommendations show that the use of Eutirox for long-term replacement therapy is safe. The severity of situations varies. Sometimes the depth of the patient's experiences does not correspond to the severity of the problem that befell him. The exception to the rule is elderly age and associated pathologies:
- adrenal insufficiency;
- inflammation of the heart muscle;
- acute myocardial infarction;
- acute inflammation of the membranes of the heart;
- atherosclerosis.
If you follow the recommendations in these cases, a dose adjustment of the drug is required. Eutirox is prescribed at 50 micrograms with further increases. Thyroxine is a hormone, and taking an artificial hormone, like taking any drug, is accompanied by side effects.

Effects of Eutirox
Eutirox is a hormonal tablet preparation that is chemically and molecularly identical to the human hormone. In case of hypothyroidism, which is accompanied by weight gain, the use of the drug leads to the fact that the function of the endocrine gland is normalized, and with good thyroxine levels, the weight is equalized. When taking a pharmaceutical product, it is possible allergic reactions, which are identified at the initial stages of admission.
As for hair loss, when taking the drug, there is an improvement in hair quality, as opposed to the effects when hair loss is a symptom of insufficient function of the endocrine gland. When the state transitions to euthyroidism, hair will stop falling out, fragility and fragility will disappear.
With an excess dose of the drug, signs of thyrotoxicosis appear - reverse state, characterized by hyperfunction of the thyroid gland. The most common ones are:
- arrhythmia;
- high blood pressure;
- insomnia;
- irritability, short temper;
- weight loss;
- hyperhidrosis;
- menstrual irregularities in women.
When the substance of the drug accumulates in the tissues of the body, changes in the work also occur. digestive system and allergic reactions.

Taking and stopping Eutirox
To avoid side effects, Eutirox must be taken correctly:
- early in the morning, usually half an hour before breakfast;
- with a small portion of plain water.
It is advisable not to skip taking the drug, but to take it constantly, at the same time, throughout the entire period indicated by the doctor. Fluctuations in hormone levels are undesirable for the thyroid gland if the drug is missed. This can lead to the growth of gland nodes. You should not take the drug in a double dose to replace the missed one - this will cause a sharp jump in function. It is advisable to take the missed dose in the morning on the same day, at lunch or in the evening.
After removal of the thyroid gland, the prescription depends on the amount of tissue removed. If part of the gland has been resected or 50% of the tissue has been removed, the need to prescribe Eutirox is determined by the tests performed. This category of patients needs to check the level of thyroxine in the blood and determine the level of thyroid-stimulating hormone. If they are within normal limits, then the use of the drug is not mandatory. If decreased gland function is diagnosed - low levels of thyroxine or, conversely, an increase in thyroid-stimulating hormone, then replacement therapy is necessary.

If the thyroid gland is completely removed, the course of treatment covers the rest of your life. When prescribing Eutirox for the purpose of blocking the production of hormones by the thyroid gland itself, as a rule, the treatment course is determined for a specific period of 1–2 months.
When planning pregnancy, it is advisable to use the Eutirox hormone in the following cases:
- if a woman has had a thyroid disease;
- if you have undergone surgery on the gland and are prescribed replacement therapy.
With hypothyroidism, pregnancy is almost impossible. Carrying out adequate therapy with the prescription of hormonal drugs is the success of the development of pregnancy. During the period of gestation, taking a hormonal drug is mandatory for those for whom it is indicated. A pregnant woman with hypothyroidism who does not take replacement medications runs the risk of giving birth to a child with signs of thyroid deficiency and mental retardation.
There are cases when it is necessary to increase the dose of Eutirox. Then the observation of such a pregnancy falls within the competence of not only the gynecologist, but also the endocrinologist. Children suffering from hormonal deficiency due to hypothyroidism also need to take this drug in the dosage and course as prescribed by a specialist. The portioned dose depends on the child’s body weight and age.
Self-discontinuation of the drug will lead to a new development of symptoms of hypothyroidism, when the production of thyroxine is impossible naturally. Cancellation of Eutirox while blocking hormonal production will not lead to pronounced changes.
Drug overdose
Taking Eutirox will bring hormone levels back to normal only in situations where it is justifiably prescribed. There is no need to be afraid of taking hormones. You need to be wary of a lack of hormones. The drug Eutirox is inexpensive, accessible and effective.
Secret zone
There is only one point to pay attention to. A normal person without signs of hypothyroidism is able to work for 3 days in a row and then recover quietly for 2 days. A person who takes the artificial hormone levothyroxine has a hard time tolerating this condition. With an active lifestyle, with increased physical and emotional stress, it is necessary high dose hormone. In case of an overdose of Eutirox in case of hypothyroidism, problems with the functioning of the heart arise during the recovery period after workload:
- increased heart rate;
- tachycardia;
- arrhythmia;
- heartache.
The effect that a hormone similar in its chemical properties has in tablets to “native” thyroxine in a state of excitement remains unknown and is being studied by medicine, as well as pharmacology. Opinions tend to favor the effect of the body processing the artificial analogue. Nevertheless, the drug fully performs its function, and the most important tasks remain nuanced. People taking Eutirox work and rest safely, reproduce and raise healthy offspring.

Combination with other dosage forms
An overdose of thyroxine or an increase in the effect of the drug may occur when consuming certain foods and dosage forms. If the dose was exceeded when taking Eutirox, the following symptoms appear:
- chest discomfort;
- dyspnea;
- convulsions;
- loss of appetite;
- disruptions in the menstrual cycle;
- sleep disturbance;
- fever and excessive sweating;
- diarrhea;
- vomit;
- rash;
- irritability.

Taking herbal infusions and vitamin complexes carried out after consultation with an endocrinologist.
The medicine becomes poison for the body when acute signs of overdose are observed, appearing within 24 hours:
- Thyrotoxic crisis, in which an increase in all signs of hyperthyroidism (thyrotoxicosis) is obvious.
- Mental disorders - convulsive seizures, delirium and semi-fainting states, leading to the development of coma.
- A sharp decrease in urine output (anuria).
- Liver atrophy.
Despite the fact that Eutirox is a drug that regulates iodine in the body, you can take iodine-containing synthetic (Iodomarin) or natural (kelp) forms. Iodomarin contains inorganic iodine, which is not produced in the body, so it must come from outside. This is especially important for pregnant women and people suffering from insufficiency of the endocrine gland.
Structural analogues
Trade analogues of the drug are represented by the names L-Thyroxin, Bagotirox, Tireotom and Novotiral. Despite the fact that all these pharmacological products have one thing in common active substance– levothyraxine, there are differences in their action. Eutirox, when taken as prescribed, unlike other structural analogues, does not have (or in rare cases has) side effects. Indicated for the treatment of childhood deficiency conditions.
Combining with other drugs, prescribing or changing the dose on your own is strictly not recommended. Only a doctor, based on physiological characteristics and individual patient health indicators, selects medicinal product, dosage and course of treatment.

First aid for overdose
When you feel the first signs of illness, you need to see a doctor or call a specialist to your home. You should not delay calling an ambulance if your condition worsens, or in the following cases:
- if an overdose occurs in a child, pregnant woman, or elderly person;
- severe heart rhythm disturbances and chest pain;
- diarrhea with bloody discharge;
- high blood pressure;
- pathologies of a neurological nature - seizures, paralysis, paresis;
- disturbances of consciousness.
Depending on the severity of intoxication, drug therapy is carried out using symptomatic drugs, blood purification procedures for unconscious patients.
 Drugs for replacement and symptomatic therapy for thyroid hypothyroidism
Drugs for replacement and symptomatic therapy for thyroid hypothyroidism
 Taking Iodomarin for reduced thyroid function
Taking Iodomarin for reduced thyroid function

What is the latent form of hypothyroidism characterized by and can it be cured?
The drug Endorm for autoimmune thyroiditis
 Features of the development and treatment of cordarone-induced thyrotoxicosis
Features of the development and treatment of cordarone-induced thyrotoxicosis
Thyroid gland: symptoms of the disease in women and principles of treatment
Unfortunately, women often encounter diseases of the thyroid gland: according to statistics, every fifth representative of the fair sex has clinically pronounced manifestations of hypothyroidism, and hyperthyroidism develops in 4-6% of the world's population. There are many causes of hormonal disorders, but each of them affects the thyroid gland: we will consider the symptoms of the disease in women + treatment of the pathology in more detail in our review and video in this article.
Clinical manifestations
All endocrine diseases of the thyroid gland are divided into two large groups:
- occurring with hypofunction (failure);
- occurring with hyperfunction (excess production of hormones).
Symptoms of thyroid disease in women can be directly opposite and depend precisely on what hormonal changes occur in the body.
With a lack of thyroid hormones, all vital processes in the body slow down.
The main symptoms of hypothyroidism include:
- bradycardia - a decrease in heart rate to 60 beats per minute or lower;
- fragility, loss of hair shafts;
- dry skin;
- constant feeling of chilliness;
- gaining excess weight with a normal diet and even decreased appetite;
- disruption gastrointestinal tract(nausea, belching, flatulence and bloating, constipation);
- increased cholesterol levels;
- fatigue, decreased performance, weakness;
- depressed mood, depression;
- menstrual irregularities, reversible infertility;
- swelling of the face and limbs;
- decreased memory, attention, and thinking abilities.
With long-term hypothyroidism, goiter may develop - an increase in the size of the thyroid gland. At the same time, the following symptoms of thyroid disease in women are added to the classic signs of hormonal imbalance: cough, difficulty breathing, shortness of breath, change or complete loss of voice caused by compression of the respiratory tract.
Note! Hypothyroidism is often diagnosed already in an advanced stage, with the development of severe multiple organ disorders. This happens because many sick people attribute the first signs of the disease to fatigue, poor health, and seasonal blues. Therefore, doctors recommend that all healthy people undergo a thyroid examination regularly (at least once every 5 years).
Hyperthyroidism
Symptoms of thyroid disease in women + treatment of pathology are directly opposite for hypothyroidism.
Characteristic signs of the disease:
- tachycardia – increased heart rate and pulse;
- arrhythmia;
- increased systolic pressure;
- thinning of skin and nails;
- heat intolerance, excessive sweating;
- weight loss despite good appetite;
- loose stools, vomiting;
- eye problems: ophthalmopathy, bulging eyes, dry cornea;
- trembling fingertips;
- insomnia, nightmares, disturbing dreams;
- nervousness and increased irritability;
- menstrual irregularities, reversible infertility.
Note! Any hormonal problems of the thyroid gland can lead to reproductive disorders in women. However, they are temporary, and after a course of treatment, menstruation is restored.
Diagnostic principles
An experienced doctor can assume a thyroid disease based on complaints and a clinical examination of the patient.
To confirm the diagnosis, the following examination must be performed:
- biochemical studies of the hormonal composition of the blood (TSH, T3, T4);
- are common clinical tests blood and urine;
- determination of antibodies to TSH and TPO receptors;
- scintaging—determining the functional activity of an organ;
- according to indications - puncture biopsy.
Treatment
Treatment of the thyroid gland - we discussed the symptoms of the disease in women above - depends on the degree of hormonal disorders. Principles modern therapy are presented in the table below.
Table: Instructions for the treatment of endocrine pathologies in women:
| Treatment Goals | Thyroid diseases with hypothyroidism | Thyroid diseases with hyperthyroidism |
| Diet | Limiting high-calorie fatty foods, soy products, and alcohol. The basis of the diet should be fruits and vegetables, seafood and lean meat | Limiting foods that stimulate the central nervous system: coffee and tea, strong rich broths, alcohol. Therapeutic nutrition should be balanced and high-calorie, as the patient quickly loses body weight. |
| Correction of hormonal imbalance | Synthetic analogues of thyroid hormones - Eutirox or L-thyroxine | Drugs that reduce thyroid activity - Mercazolil, Tyrosol, Metizol |
| Radical therapy (if drug treatment is ineffective) | An operation to remove an endocrine organ is used when there is a significant increase in its size and the formation of a grade 4-5 goiter. | Surgical removal of the organ. “Switching off” the thyroid gland from working using radioactive isotopes of iodine. |
Do-it-yourself folk methods for treating thyroid pathology (vegetable juices, preparations based on white cinquefoil, European grasshopper, gorse, etc.) only briefly eliminate the symptoms of hormonal disorders, but do not combat their causes.
Note! Patients who have undergone surgery to remove the thyroid gland are forced to take hormonal medications throughout their lives.
The sooner endocrine pathology is diagnosed, the more effective its therapy will be. It is important to begin treatment for thyroid disease as early as possible: symptoms in women, although they develop slowly, are quite typical and are not difficult to diagnose.
Complications of hypothyroidism and hypothyroid coma
 Hypothyroidism is a dysfunction of organs and systems caused by low functionality of the thyroid gland. Reduced synthesis of gland hormones causes various symptoms and disruption of internal organs.
Hypothyroidism is a dysfunction of organs and systems caused by low functionality of the thyroid gland. Reduced synthesis of gland hormones causes various symptoms and disruption of internal organs.
The disorder often occurs in middle-aged women, but can also develop in men who have had an endocrine gland removed.
After prescribing replacement therapy, the patient has the opportunity to live a full life; the prognosis in this case is favorable, life expectancy is quite high.
Complications of hypothyroidism occur in the absence of treatment, the quality of life drops sharply, this is especially true for older people. They often die from cardiac and respiratory failure. In some cases, it is not possible to save lives even with timely and correct therapy, even for people under 30 years of age.
- Clinical picture of hypothyroidism
- Diagnostic measures when examining patients with hypothyroidism
- Hypothyroid coma
- Emergency care for hypothyroid coma and subsequent treatment of complications
- Nuances emergency care with severe consequences of hypothyroidism
- Treatment of complications of hypothyroidism in children
Clinical picture of hypothyroidism
 Can hypothyroidism be cured and how long will it take for symptoms to subside? It all depends on the age of the patient, the cause of the disorder and its severity. Treatment may take several years, and in some cases treatment will take a lifetime.
Can hypothyroidism be cured and how long will it take for symptoms to subside? It all depends on the age of the patient, the cause of the disorder and its severity. Treatment may take several years, and in some cases treatment will take a lifetime.
The severity of symptoms increases gradually; at the very beginning, health problems do not bother patients. Most often, this picture occurs in patients after removal of part of the gland. The resulting condition is called postoperative primary hypothyroidism.
Symptoms of thyroid hypothyroidism:
- chilliness;
- depression;
- unreasonable weight gain;
- constant fatigue;
- problems with the cardiovascular system;
- baldness;
- pale skin;
- insomnia;
- elevated cholesterol levels;
- disturbance of attention and thinking.
Diagnostic measures when examining patients with hypothyroidism
 If hypothyroidism is suspected, the patient is asked to undergo laboratory tests for thyroid hormones. The TSH level is indicative; its normal level excludes hypothyroidism.
If hypothyroidism is suspected, the patient is asked to undergo laboratory tests for thyroid hormones. The TSH level is indicative; its normal level excludes hypothyroidism.
Mistakes can occur in diagnosing hypothyroidism, as its symptoms can be disguised as other diseases.
A decrease in thyroid function in patients over 50 years of age is considered a sign of aging, since the following symptoms: dementia, general weakness, poor appetite, dry skin, high cholesterol are typical for older people. In children, decreased functionality of the gland may be congenital and may not appear during the first years of life.
The set of diagnostic measures includes:
- visual inspection;
- palpation of the thyroid gland;
- gland biopsy;
- lab tests.
Hypothyroid coma
 Hypothyroid coma affects people after surgery on the gland, injuries, overdose of narcotic and sedative drugs, hypothermia.
Hypothyroid coma affects people after surgery on the gland, injuries, overdose of narcotic and sedative drugs, hypothermia.
GC are characterized by:
- hypoxia of internal organs;
- hypoventilation of the lungs;
- bradycardia;
- low body temperature;
- hypoglycemia;
- high cholesterol.
Lack of adequate medical care leads to death.
Symptoms of GC:
- drowsiness;
- severe depression;
- body temperature up to 35°;
- skin is cold;
- suppression of reflexes;
- low pressure;
- disruption of the central nervous system.
 Tachycardia in hypothyroidism increases with the onset of coma and is the cause of death of the patient.
Tachycardia in hypothyroidism increases with the onset of coma and is the cause of death of the patient.
Arrhythmia is caused by a decrease in the number of β-adrenergic receptors, while norepinephrine is produced intensively, which causes spasm of the coronary arteries and heart failure.
Emergency care for hypothyroid coma and subsequent treatment of complications
- With immediate medical attention, the prognosis for GC will be positive, especially for patients under 30 years of age. The patient is administered hydrocortisone, the daily dose of the drug should not exceed 200 mg, as well as thyroxine drip, the daily dose of thyroxine is up to 500 mg.
- In especially severe cases, blood transfusions and artificial ventilation of the lungs are performed, after which glucocorticoids are administered.
- To prevent infectious complications, antibiotic therapy is carried out.
- For atony Bladder a urinary catheter is inserted.
 After emergency treatment, treatment with special drugs begins. Hypothyroidism can be treated with an individually adjusted dose of the synthetic hormone thyroxine.
After emergency treatment, treatment with special drugs begins. Hypothyroidism can be treated with an individually adjusted dose of the synthetic hormone thyroxine.
The use of thyroxine improves the patient’s quality of life and promotes its duration.
 For the treatment of thyroid hypothyroidism, Eutirox is prescribed once a day, before breakfast. It is recommended to drink the drug with clean boiled water. The initial dose is 50 mcg, gradually increased to 200 mcg.
For the treatment of thyroid hypothyroidism, Eutirox is prescribed once a day, before breakfast. It is recommended to drink the drug with clean boiled water. The initial dose is 50 mcg, gradually increased to 200 mcg.
The dosage is increased every three weeks until the patient reaches a euthyroid state of the gland. If there is no effect from treatment, malabsorption or improper administration of the drug may be suspected.
An adequate dose allows you to get rid of symptoms and improve your quality of life within two months.
Basics  The main criteria that determine treatment tactics are the duration of thyroid dysfunction and the severity of symptoms. The effectiveness of therapy is proven by the disappearance clinical symptoms And clinical diagnostics. The longer the duration of uncompensated disruption of the gland, the less time the patient has to live, even after starting therapy.
The main criteria that determine treatment tactics are the duration of thyroid dysfunction and the severity of symptoms. The effectiveness of therapy is proven by the disappearance clinical symptoms And clinical diagnostics. The longer the duration of uncompensated disruption of the gland, the less time the patient has to live, even after starting therapy.
In order to avoid the serious consequences of endocrine gland disease, people over 30 years of age are recommended to undergo preventive examinations at least once a year. This will allow you to live, maintaining health and activity for a long time, since in many ways these factors largely depend on the synthesis of thyroid hormones.
Nuances of emergency care for severe consequences of hypothyroidism
All measures to provide assistance to patients with hypothyroid coma are carried out in the intensive care unit. During therapy, it is necessary to increase the level of hormones of the endocrine gland, eliminate hypothermia, problems with the heart and blood vessels, and normalize the nervous system.
 For this by drip Levothyroxine is administered; it can also be administered intramuscularly.
For this by drip Levothyroxine is administered; it can also be administered intramuscularly.
For people over 30 years of age, the rate of levothyroxine required to achieve optimal thyroid condition is 1.9 mcg/kg per kilogram of body weight. For older people, the dose of the synthetic hormone is slightly less, up to 1 mcg/kg.
How much levothyroxine can pregnant women take to relieve severe conditions? In such cases, the dosage is prescribed individually and adjusted depending on the trimester of pregnancy.
Hypothyroidism after menopause in women is corrected with increased doses of hormones, laboratory tests are carried out every two months, especially for women who have had part of the thyroid gland removed.
Basic manipulations aimed at eliminating HA and its consequences:

Treatment of complications of hypothyroidism in children
Complications of hypothyroidism in children occur in rare cases when treatment after removal of part of the gland or in the case of congenital hypothyroidism is carried out incorrectly or not at all. In especially severe cases, irreversible changes called cretinism develop, as well as dwarfism, delayed physical development, partial damage to the central nervous system.
 Congenital thyroid deficiency in children or acquired as a result of surgery is corrected with synthetic hormones, but in some cases the symptoms (poor memory, high cholesterol, chilliness, decreased cognitive abilities, poor bowel function, depression) persist. This happens if the dose is small or the drug is poorly absorbed by the intestines. The effectiveness of thyroxine is also reduced by drugs such as ferrous sulfate and calcium; in such cases, the dosage of hormones is increased.
Congenital thyroid deficiency in children or acquired as a result of surgery is corrected with synthetic hormones, but in some cases the symptoms (poor memory, high cholesterol, chilliness, decreased cognitive abilities, poor bowel function, depression) persist. This happens if the dose is small or the drug is poorly absorbed by the intestines. The effectiveness of thyroxine is also reduced by drugs such as ferrous sulfate and calcium; in such cases, the dosage of hormones is increased.
Help, no one knows what to do. Thyrotoxicosis and its background tachycardia and hypertension since 2014. I took ACE, calcium blockers - it didn’t help. Doctors couldn't find a reason. On June 10, 2018, an attack of atrial fibrillation, a blood pressure of 180/70, beta-blockers were prescribed - it helped relieve tachyardia (the pulse was constantly about 100), she took cardoron and it relieved the pain in the heart, but on June 20, another attack of arrhythmia and pressure, Besedov’s disease was discovered: T4 - 64, TSH - 0.01, AT to TG - 5, cholesterol 2.6. On June 22, I started taking tyrosol 30 mg. , beto-blockers bisoprolol 5 mg, but they did not help relieve heart pain, despite the fact that they relieved tachycardia and even drove me into bradycardia: I had constant heart pain, insomnia, so I took cardarone myself - it helped relieve heart pain. I took Cardoron for 3 days, 200 mg. In general, I ate about 10-15 tablets. A week later, the blood pressure increased - 200/80; tyrosol was increased to 40 mg. for 2 weeks, then again 30 After that I felt good for a month and a half. after 2 months in August: T4 - 20 TSH - 0.05 Symptoms of hypothyroidism began: persistent constipation, urine did not work (I went to the toilet drop by drop), I gained weight, depression, 50% of my hair fell out in a week, my pulse began to drop to 40 in the evening. But he was not particularly high before on beto blockers: about 50. Tyrosol was reduced to 10-20 mg. My blood pressure is normal 110/70. I decided to take l-thyroxine 50 mg. Immediately I felt better: my stool improved and a diuretic effect appeared. A surge of energy appeared, depression went away, and even sex appeared, which was not there as soon as “hypothyroidism” appeared. But after 5 days, the hot flashes and thyroxine were canceled, and after another 2 days - an attack of tachycardia - about 160 beats. per minute + atrial fibrillation, removed myself with cardon. Took tests: T4 - 14 TSH - 0 Cholesterol 4.6 tyrosol was prescribed 15 mg. Although I had not taken L-thyroctine for 2 weeks, my condition was getting worse every day: every day I had attacks (in the evening) of high blood pressure, and the beto-blockers stopped working! They only made things worse: attacks of hypertension an hour after taking the blockers. pulse 45. Symptoms of cerebrovascular accident began: attacks of partial loss of vision, flashing of bright light during attacks of pressure, which were not there before. The pressure is not like with theriotoxicosis (high upper and normal lower, but high both upper and lower). Heart pain began, as before with thyrotoxicosis. I was taken to the hospital by the doctor there who prescribed 30 mg of tyrosol. Pain in the heart and liver. On ultrasound, the liver and gall bladder are diffuse, which was not the case 3 months ago. Bronchospasm. The condition 3 weeks after stopping L-thyroxine became critical: attacks of pressure surges became more frequent and occurred 5 times a day. I removed it with a hood because the beto-bloators did not work. The doctors didn't know what to do. I took tests: T 4 - 9 feretin - normal cortisol - normal I decided to take the risk of taking l-thyroxine in a smaller dose of 30 mg, to cancel all beto-blockers and all blood pressure pills. Tyrosol was temporarily reduced to 5 mg. The attacks of high blood pressure went away, the pulse returned to normal to 55-65, the signs of cerebral circulation disorders disappeared, even the hair stopped growing, although the skin became drier, dried out and cracked around the nails, but a week later, when taking the next dose of only 30 mg of “kerosene” - tachycardia 140. I took it off with a beto blocker. I stopped taking L-thyroxine (kirosine). The pressure was normal. It became very cold. I couldn’t go outside: my muscles were inflamed from the cold here and there, although I dressed warmly, and I was constipated. After 5 days, attacks of high blood pressure began again in the evening, again taking a dose of “kirosine” at night. 30 mg - in the morning tachycardia 140 and high pressure 160/90. Despite the tachycardia, today I again took a dose of “kirosine” 30 mg. My heart and liver don't hurt yet. What to do? I feel like I have hypothyroidism.